THIS CONTENT IS BROUGHT TO YOU BY SINTEF - read more
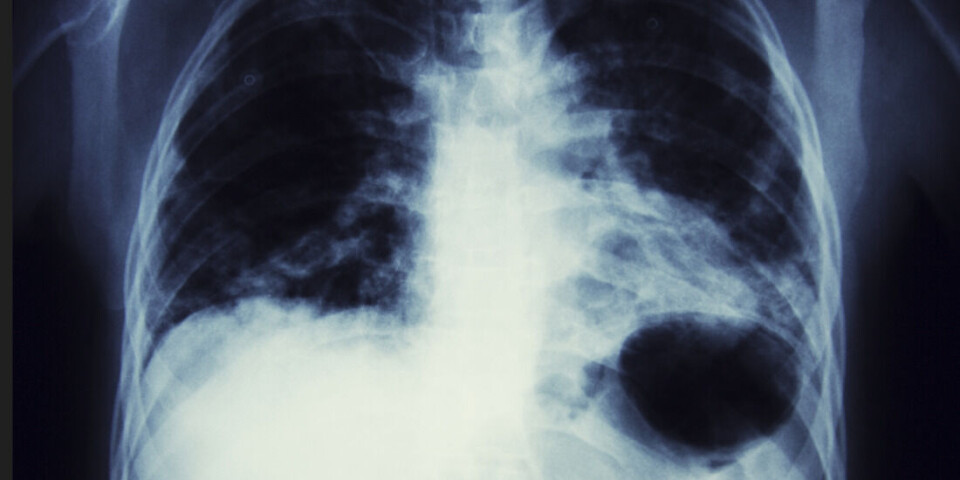
Experiments on mice: Nanomedicine using gas bubbles may offer a new cure for lung cancer
The gas bubbles deliver chemotherapy directly into the lungs.
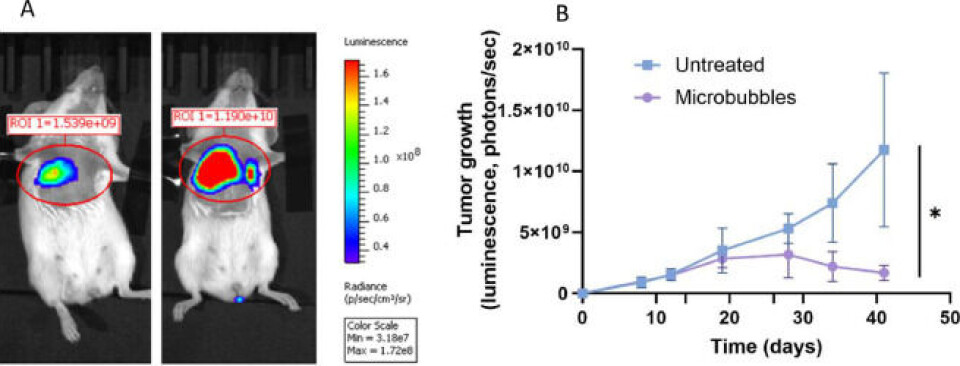
Results from experiments with mice have shown that the impact of this form of medication is very great.
Tumours were significantly reduced in size after only 30 days following the start of treatment.
The method is so promising that the research team from SINTEF has taken out a patent. They have also signed a licence agreement with a pharmaceutical company.
“We’re very confident that this approach may offer us a new cure for lung cancer,” says researcher and project manager Andreas Åslund. He works at SINTEF’s Department of Biotechnology and Nanomedicine.
From a drawback to a benefit
It was in many ways something of a coincidence that this technology should end up as a lung cancer medication.
Originally, the research team was working to identify a method that would deliver drugs to the brain. This is particularly difficult because the brain is enclosed in a separate membrane called the blood-brain barrier.
In other words, methods other than delivering drugs via the bloodstream are required in order to reach brain tumours. The researchers have addressed this problem by manufacturing gas bubbles that enclose the nanocapsules containing the drugs.
The bubbles make it possible to use ultrasound to explode the nanocapsules, enabling the drugs to be ‘shot’ through the blood-brain barrier.
So, at what scale are the researchers actually working?
This is nanoscale – so small that as many as 100 nanocapsules, containing the drugs and enclosed in their gas bubbles, can sit across the width of a human hair. This being said, the drug itself constitutes only ten per cent of the package.
“After a while, we discovered that these gas bubbles ended up in the patients’ lungs. In the first instance, an accumulation of gas bubbles here wasn’t what we wanted. But the discovery meant that we could turn the problem upside down and instead exploit the phenomenon to reach tumours in the lungs,” explains Åslund.
Into the capillary network
The reason that this medication is so well suited to treatment of the lungs is that it takes place at nanoscale.
All intravenous drugs enter the bloodstream and pass through the heart before they reach the lungs, where the vessels develop into what is called the capillary network. Here, the vessels are very narrow and act as a filter for the microbubbles, which explode spontaneously and so deliver the nanoparticles containing the drugs directly into the lung tissue.
Because the bubbles burst spontaneously, there is no need to use ultrasound to free the nanoparticles from their capsules in the capillary network.
Many years of research
The idea for this very specific form of medication emerged in the same department at SINTEF as early as 2014.
A decade of research work has led to many medicinal innovations. These include a drug delivery platform for the treatment of peritoneal cancer, which resulted in the spin-off company NaDeNo. And today, a new cure for lung cancer is on the researchers’ agenda.
Delivering drugs at nanoscale means that treatment is more gentle on the patient.
“Nanomedicines have the benefit of acting very locally. This makes it possible to treat only the diseased tissue, and also enables us to administer stronger drugs. In so doing, we don’t have to worry about the drugs damaging healthy tissue. It also means that the patient will not suffer as many side-effects. It would in fact be very dangerous to administer drugs of this efficacy if the doses weren’t so minute,” the researcher says.
This technology makes it possible to deliver more than just cancer drugs to the lungs.
“We envisage that this method of drug delivery can also be used to treat other lung conditions such as cystic fibrosis, infections and pulmonary emphysema,” says Åslund.
Reference:
Snipstad et al. Nanoparticle-loaded microbubbles for treatment of lung cancer, European Journal of Pharmaceutical Sciences, vol. 199, 2024. DOI: 10.1016/j.ejps.2024.106804
———
Read the Norwegian version of this article on forskning.no
More content from SINTEF:
-
300 meals can be saved from this kitchen – every month
-
Saving seagrass and French oysters: New solutions give new life to Europe's coastal areas
-
What does ultra-processed food do to our gut flora?
-
This new device can make it cheaper to heat your home
-
Propellers that rotate in opposite directions can be good news for large ships
-
How Svalbard is becoming a living lab for marine restoration





































