THIS ARTICLE/PRESS RELEASE IS PAID FOR AND PRESENTED BY University of Oslo - read more

Can predict cognitive impairment after stroke
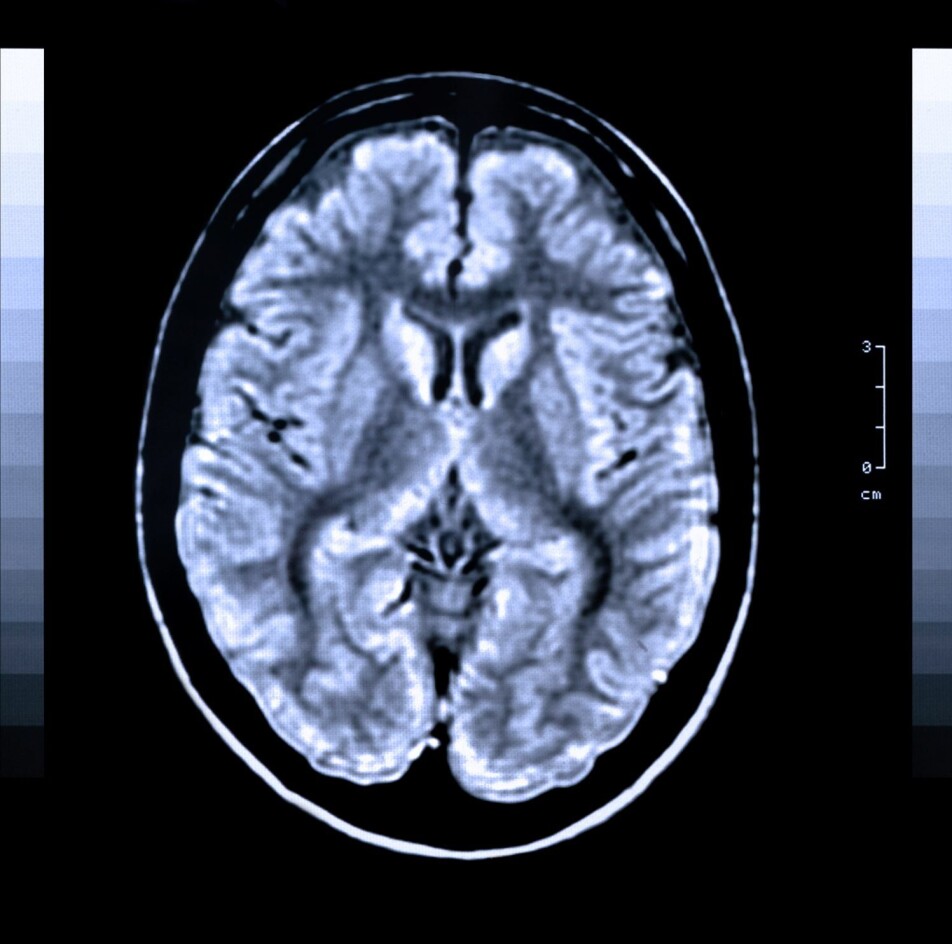
Researchers in the Nor-COAST study used MRI images of stroke patients’ brains to identify those who may develop cognitive impairment after the stroke.
Stroke is caused by disturbances in the blood circulation of the brain due to blood clots or cerebral haemorrhage. This causes damages to parts of the brain and the patient experiences a sudden loss of particular body functions. Individuals affected by stroke need urgent, life-saving treatment followed by rehabilitation. In Norway, stroke affects approximately 12,000 people each year.

“It appears that about 50 percent of stroke patients get some form of cognitive impairment after the stroke,” says Till Schellhorn, who has written his doctoral thesis at the Institute of Clinical Medicine based on the Nor-COAST study.
Cognitive impairment means that an individual’s ability to think and to perform intellectual and mental processes has been reduced.
Can identify at-risk patients using MRI images
The researchers examined the brains of patients who developed cognitive impairment after stroke using MRI images. MRI stands for magnetic resonance imaging, and is a method used to take pictures of the body's internal organs.
“Using MRI images of the brain, we can identify risk patients for the development of cognitive impairment after stroke with good certainty,” says the researcher.
The MRI images showed that patients who develop cognitive impairment after stroke already had brain changes prior to the stroke that may be associated with the development of cognitive impairment.
“It was mainly the case for patients with small vessel disease, who have a reduced circulation in the small blood vessels in the brain. This can lead to many small cerebral infarctions, and was associated with the development of cognitive impairment after stroke,” Schellhorn explains.
Furthermore, the results showed that the size of the stroke was associated with increased risk of developing cognitive impairment. The larger the stroke, the higher the risk of developing cognitive impairment afterwards.
There was also an association between loss of substance in the temporal lobe, which is a part of the brain associated with memory, and the development of cognitive impairment.
“But this association was less pronounced than we had expected,” he points out.
Has put cognitive impairment after stroke on the agenda
“The Nor-COAST study has put cognitive impairment after stroke on the agenda. In the past, the focus has mostly been on paralysis and other physical ailments, and therefore cognitive impairment has received little attention,” Schellhorn explains, and adds:
“But cognitive function means a great deal for the quality of life, both of the patient and their families.”
The researchers have set themselves the goals of contributing to more knowledge about the causes of cognitive impairment and developing methods for identifying at-risk patients.
“You have to know whom, and why the individual patient develops cognitive impairment in order to be able to start a treatment,” he points out.
Aim for better preventive measures and treatment
“We hope that our research can lead to better treatment of cognitive impairment after stroke in the future. We hope that we can prevent and alleviate cognitive impairment,” Schellhorn says.
The researchers are now testing potential preventive measures and novel forms of treatment.
“This could entail preventive treatment among stroke patients with a high risk of developing cognitive impairment, or treatment of the causes, such as cardiovascular disease,” the researcher elaborates.
Schellhorn further states that increased physical or social activity as part of rehabilitation after a stroke might slow down the development of cognitive impairment.
Made a model for clinical use
Eight hundred and fifteen stroke patients were included in the study. The researchers took MRI images of the brain of 410 of them.
The researchers examined these images thoroughly. On the MRI images, which were taken after the stroke, they could see which patients had changes in the brain that had been present already prior to the stroke. To do this, they used different types of MRI images, some that show that brain changes are acute and some that show brain changes of older date.
“It is a combination of specific MRI technique and interpretation that helps us say something about the age of the brain changes,” Schellhorn points out.
The researchers believe that some of these changes in the brain were related to the development of cognitive impairment after stroke.
“We investigated the association between the image findings and cognitive impairment. We created a model for predicting the risk of cognitive impairment based on the findings on the images,” Schellhorn explains.
So far, the model has only been tested within the scope of the Nor-COAST study, but the researchers already have plans to test it on more stroke patients. However, there are also a number of practical challenges that must be solved before the model can be used in a clinical context, i.e. for use in connection with the treatment of patients.
“Before using new computer programmes at the hospital, the models must go through a routine security check. Such things typically take some time, the researcher says,” and adds:
“But I hope that we can use our models in the clinic at the hospital over the next two to three years.”
Reference:
Eva Birgitte Aamodt et.al.: Predicting the Emergence of Major Neurocognitive Disorder Within Three Months After a Stroke. Frontiers in Aging Neuroscience, 2021.
———
Read the Norwegian version of this article at forskning.no
See more content from the University of Oslo:
-
Mainland Europe’s largest glacier may be halved by 2100
-
AI makes fake news more credible
-
What do our brains learn from surprises?
-
"A photograph is not automatically either true or false. It's a rhetorical device"
-
Queer opera singers: “I was too feminine, too ‘gay.’ I heard that on opera stages in both Asia and Europe”
-
Putin’s dream of the perfect family





































