THIS ARTICLE/PRESS RELEASE IS PAID FOR AND PRESENTED BY SINTEF - read more
A tiny liver or a minuscule heart can now grow on a microchip
This connection opens up unprecedented research opportunities.
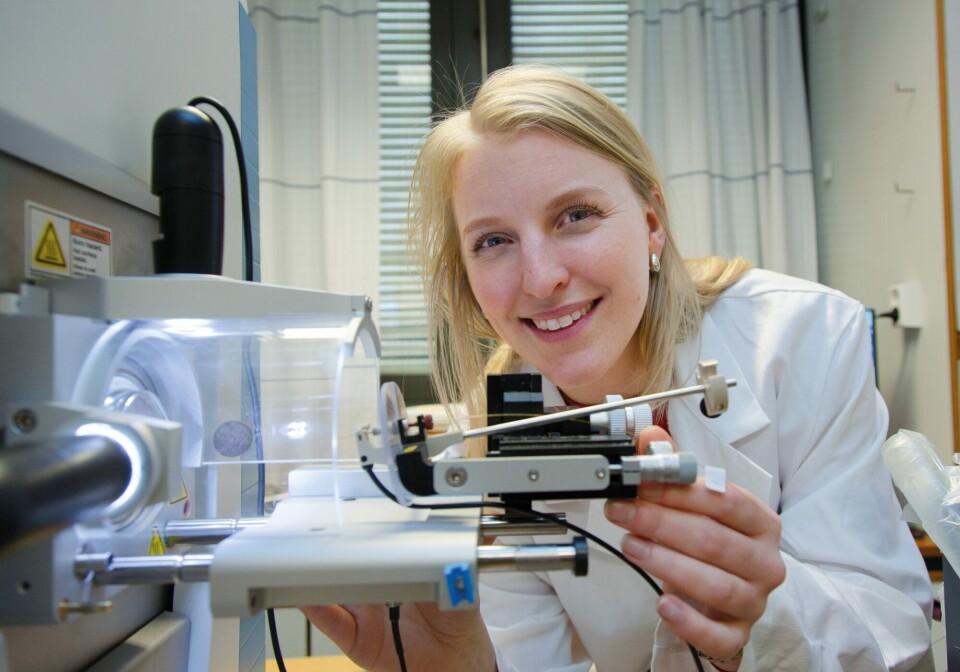
“This technology enables us to study and simulate such processes as embryonic development and the menstrual cycle, or the way in which a cancer spreads. And not least, it is expected to drastically reduce our reliance on animal testing,” SINTEF researcher Frøydis Sved Skottvoll says.
It all started with the Japanese research scientist Shinya Yamanaka, who revolutionised the world of stem cell research when he succeeded in reprogramming a skin cell back into a stem cell.
This approach suddenly made stem cells universally accessible and earned Yamanaka the Nobel Prize for Medicine in 2012.
Grows small mini-organs
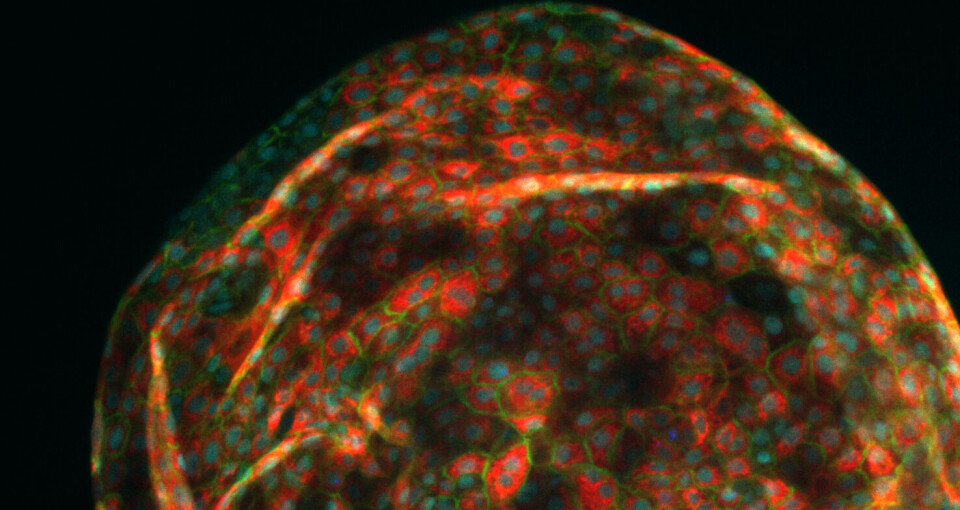
Some years later, researchers succeeded in using stem cells as the starting point for growing the first mini-organs. Today, such organs are known as organoids.
Efforts are now being made to advance the technology – more specifically, the aspect of the technology that addresses the microsystem within which these organoids are studied.
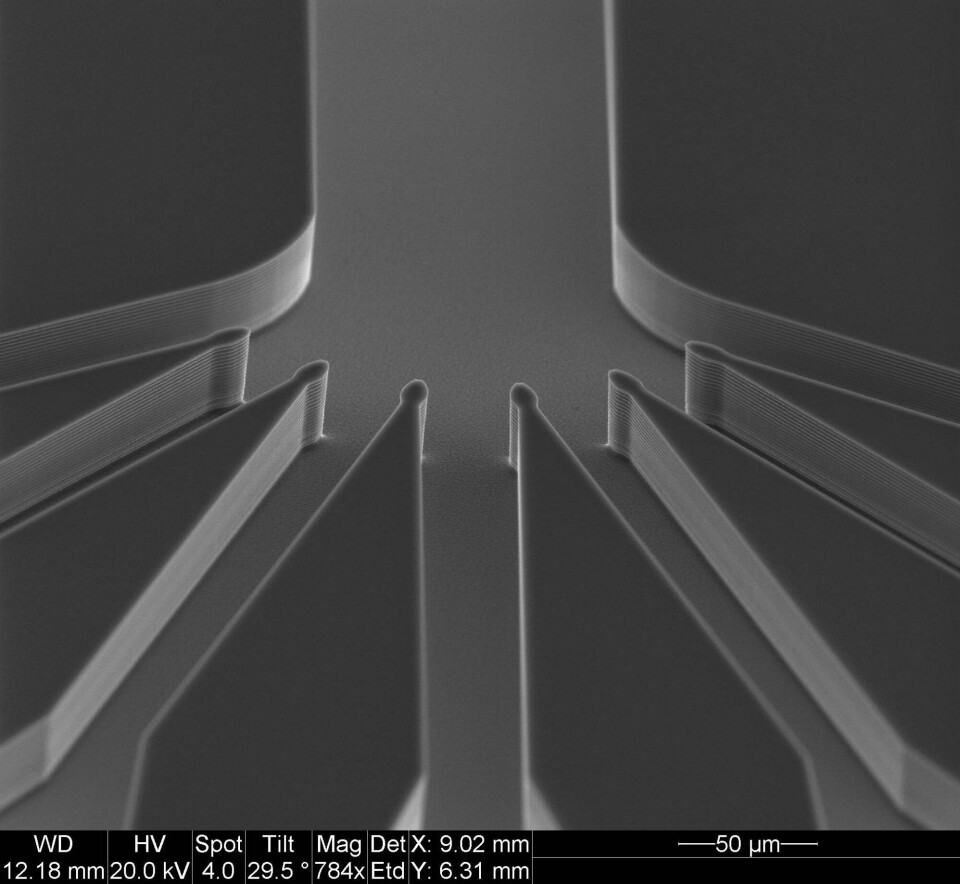
“We do this by utilising fabrication methods developed by the microchip industry to make tailored microchannel networks and sensors that can simulate processes taking place in the body. We’re also able to measure how the organoids function within the microsystem,” the researcher says.
What exactly is ‘organ-on-a-chip’?
The technology consists of two elements – an organoid, cultivated from a stem cell and a tiny three-dimensional chip made up of a network of minute microfluidic channels separated by a membrane.
Researchers can introduce a variety of molecules into the channels that provide the cells with different signals, which in turn influences fluidic flow through the cells.
The membrane acts as a porous, dividing wall that enables the molecules to diffuse, or be transported, between two different organoids, somewhat like the action of a blood vessel.
The aim here is to simulate the biological processes that take place at the cellular level within the body.
Skottvoll explains that the technology can also be used to simulate, for example, what is called the blood-brain barrier. This is the body’s fail-safe mechanism that prevents unwanted substances from passing between the brain and our bloodstream.
"Our brains are deliberately separated from our circulation system, which in the first instance is a good thing. However, it can be a disadvantage in situations where we may want to medicate the brain,” she says.
It has traditionally been very difficult to study this function in humans. However, the organ-on-a-chip technology has now made this possible.
What is a stem cell?
As well as having a microstructure that mimics biological processes at cellular level, we also need a stem cell that can act as a ‘seed’ for the entire process. But what exactly is a stem cell?
According to the Norwegian Biotechnology Advisory Board, stem cells constitute the starting point for all the cells and tissues in our bodies. They are also responsible for tissue maintenance and the repair of damaged tissue.
Stem cells have the unique ability to regenerate and divide over prolonged periods. They can also develop into more specialised cells by means of a process called cell differentiation. In this way, a stem cell can act as a ‘parent’ to everything from blood cells to muscle cells. However, a stem cell can never develop into an egg or sperm cell.
“Once we know what we want to do, it’s a bit like making sourdough: On day one, you complete the first step. On day two, you do something else, and then follows a lot of stirring and waiting until eventually you can add more ingredients. And so it goes on until we are satisfied that the cells have developed into an organoid. Sometimes, they will even develop into the same shape as a real organ,” Skottvoll says.
Organoids can provide us with many answers
Skottvoll became interested in organoid technologies at an early stage in her career. As a doctoral student at the University of Oslo, she began working with organ-on-a-chip.
She was able to observe exactly how much a ‘mini-liver’ resembles a real organ when exposed to a variety of medications.
“What I found was that they behave in a very similar way to human livers,” she says.
However, they respond more slowly than real organs when it comes to breaking down drugs. In practice, this means that experiments using such organoids may take time because they are not ‘fully’ developed.
"We believe that the reason for this is that organoids have not yet been developed with a vascular system that can transport drugs internally,” the researcher says.
Can simulate anything
The physical basis for organ-on-a-chip is a microscopic structure consisting of membranes and a network of microfluidic channels. It is these microstructures that are now being created at the SINTEF MiNaLab.
“ Just as important as creating an organ-on-a-chip is measuring what actually happens. For this reason, we’re also developing sensor technology that automatically monitors how the organoids are functioning on their chips,” Skottvoll says.
Goodbye to animal testing and more rapid drug development?
In the future, animal testing may become unnecessary. We may also be able to cultivate organs instead of relying on organ donors. Furthermore, we can test treatment methods and medications on ‘real’ human organs.
It is in fact possible even today to run advanced simulations of cell behaviour such as ‘in vitro’ embryo development – conducted entirely in a cell culture in a laboratory.
“Naturally, this is a field that raises a number of issues in terms of research ethics. Research into human brain organoids is a particularly hot topic these days,” Skottvoll says.
More personalised medicine
However, there is no doubt that this is a technology that can be used to provide us with more effective treatment methods, not least in the field of what is known as personalised medicine.
According to Skottvoll, this will change the way in which we select patient treatments.
She explains that if a patient has liver cancer, it will be possible to grow a patient-specific mini-liver and use organ-on-a-chip technology to simulate how different treatments and medications affect the cancer and the patient's liver.
“We will thus avoid having to test ineffective drugs on the patient, and the patient will avoid having to suffer any person-specific side-effects of the drugs,” Skottvoll says.
See more content from SINTEF:
-
Saving seagrass and French oysters: New solutions give new life to Europe's coastal areas
-
What does ultra-processed food do to our gut flora?
-
This new device can make it cheaper to heat your home
-
Propellers that rotate in opposite directions can be good news for large ships
-
How Svalbard is becoming a living lab for marine restoration
-
New study: Even brand-new apartments in cities can have poor indoor air quality





































