THIS CONTENT IS BROUGHT TO YOU BY University of Oslo - read more
Could this new approach help combat antibiotic-resistant respiratory infections?
“The nasal microbiota acts as a first line of defence. When this balance is disrupted, it can pave the way for inflammation and infection. Restoring this balance is key,” says researcher.

The nasal passages are home to a diverse microbial community that includes a mix of bacteria, viruses, and fungi.
In healthy individuals, this microbiota helps protect against illnesses. But when this balance is disturbed –called 'dysbiosis' – it can lead to conditions like CRS. Research shows that dysbiosis often involves an overgrowth of potentially harmful bacteria, like Staphylococcus aureus or Haemophilus influenzae, and not enough beneficial microbes.
“The nasal microbiota acts as a first line of defence. When this balance is disrupted, it can pave the way for inflammation and infection. Restoring this balance is key,” says Fernanda Petersen.
She is a professor at the University of Oslo's Faculty of Dentistry.
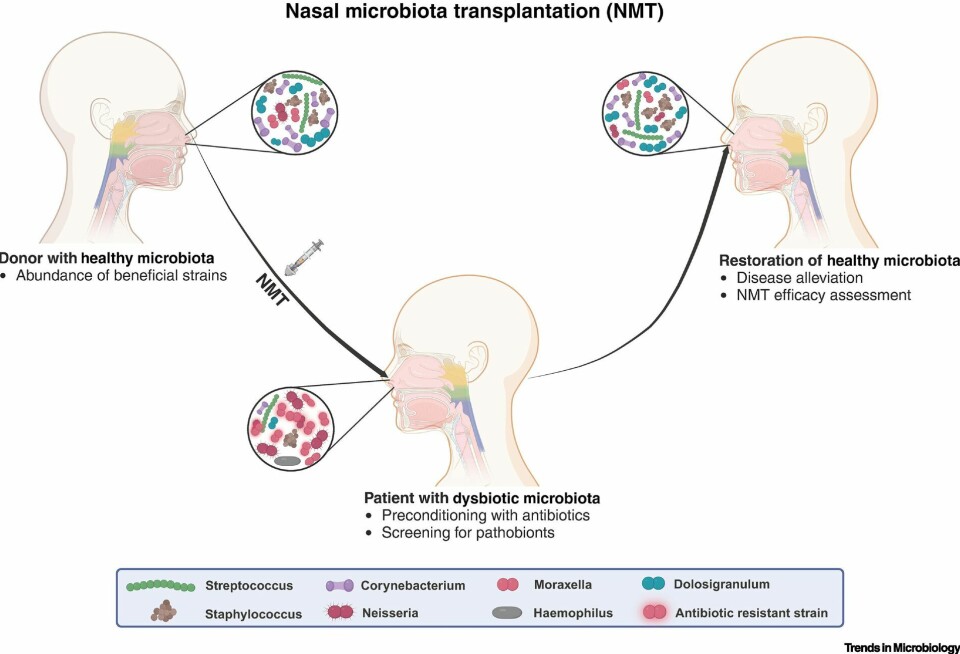
Microbiota transplantation is a procedure where microbial communities from healthy donors are transferred to patients with conditions like Clostridioides difficile infections, using faecal material. It builds on our understanding of microbial ecosystems and their impact on human health.
Recently, this concept was tested in studies using nasal microbiota for the treatment of chronic rhinosinusitis (CRS).
“The concept of nasal microbiota transplantation is groundbreaking. While it has been tested for CRS, it may find future applications in managing respiratory infections and antimicrobial resistance," she says
Petersen has contributed to a perspective article on nasal microbiota transplantation (NMT).
Early success with NMT in CRS
CRS affects millions, causing persistent inflammation in the sinuses.
Standard treatments like antibiotics, steroids, and surgery often provide only temporary relief. Recent research suggests NMT could offer a long-term solution.
In one Swedish trial, CRS patients received donor nasal microbiota after a course of antibiotics. Three months later, they had fewer symptoms and greater microbial diversity. However, some patients experienced mild side effects like fever or sinusitis-like symptoms.
Petersen notes that these results are promising, but larger, controlled studies are needed to fully understand the benefits and risks.
Combating antibiotic resistance
The rise of antibiotic-resistant microbes is a growing concern.
The nasal cavity, home to pathogens like Streptococcus pneumoniae and Staphylococcus aureus, plays a key role in their spread. NMT could help restore a healthy microbiota, pushing out resistant strains and reducing the need for antibiotics.
“This is where NMT could have a game-changing impact. By fostering a competitive environment, we may limit the colonisation of resistant microbes, promoting a healthier microbial balance,” says Petersen.
“Antimicrobial resistance is a global challenge, and exploring alternative approaches like NMT is crucial," says Achal Dhariwal.
He is a postdoctoral fellow at the University of Oslo and has contributed to the study.
Dhariwal argues that a better understanding of microbial interactions could help reduce dependence on traditional antibiotics.
Challenges and future directions
While promising, NMT faces hurdles.
Screening donors to prevent pathogen transmission is essential. However, long-term safety and efficacy data are still lacking. Synthetic microbiota – engineered communities of beneficial microbiota – could offer safer alternatives, but their development is still in early stages.
“One exciting avenue is the use of prebiotics – compounds that promote beneficial microbes – and microbial metabolites, which are health-boosting substances produces by these microbes, to support beneficial nasal microbes,” suggests Petersen.
“This could complement NMT or even replace it in certain cases,” she says.
The path ahead might involve refining NMT protocols, addressing regulatory guidelines, and investigating its uses in other respiratory conditions.
Changed to get the right nuance. It is not that researchers aim, but that is what I foresee ahead.
Preclinical models, such as germ-free animals with specific microbiota, could help uncover the mechanisms behind its therapeutic effects.
Looking ahead
“NMT is more than just a novel therapy. It represents a paradigm shift in how we approach respiratory health,” says Petersen.
For years, faecal microbiota transplantation (FMT) has been used to combat recurrent Clostridioides difficile infections, with remarkable success. By applying insights from FMT, researchers hope to unlock the full potential of the nasal microbiota.
“We are at the forefront of an exciting era. If successful, NMT could revolutionise treatment for CRS and AMR infections, offering new hope for patients worldwide,” she concludes.
Reference:
Shekhar et al. Nasal microbiota transplantation: a gateway to novel treatments, Trends in Microbiology, 2025. DOI: 10.1016/j.tim.2024.12.010

This content is paid for and presented by the University of Oslo
This content is created by the University of Oslo's communication staff, who use this platform to communicate science and share results from research with the public. The University of Oslo is one of more than 80 owners of ScienceNorway.no. Read more here.
More content from the University of Oslo:
-
Mainland Europe’s largest glacier may be halved by 2100
-
AI makes fake news more credible
-
What do our brains learn from surprises?
-
"A photograph is not automatically either true or false. It's a rhetorical device"
-
Queer opera singers: “I was too feminine, too ‘gay.’ I heard that on opera stages in both Asia and Europe”
-
Putin’s dream of the perfect family




































