THIS CONTENT IS BROUGHT TO YOU BY NTNU Norwegian University of Science and Technology - read more

Cholesterol type can affect your heart attack risk
Researchers are searching for markers that can reveal the risk of a heart attack before a patient falls ill.
Vascular plaque. It starts with inflammation. Perhaps your blood pressure has been a little too high for a little too long, putting strain on your blood vessels.
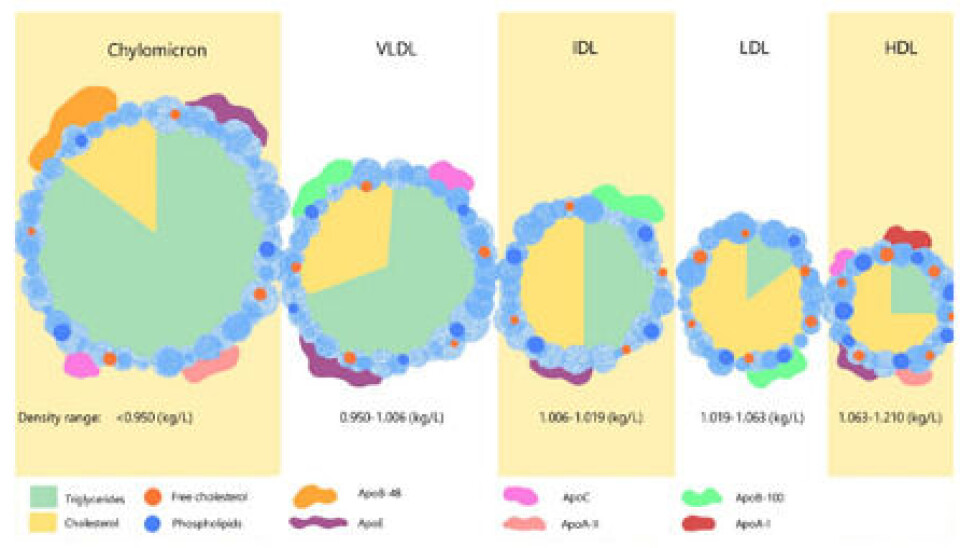
Small particles called lipoproteins, which contain cholesterol, attach themselves to the artery wall and are attacked by immune cells. A lump of fat and dead cells builds up under a thin, protective membrane.
This lump remains invisible to the naked eye, until one day it completely blocks the blood vessel. Or until it suddenly bursts. Oxygen is unable to reach the heart, resulting in a heart attack.
“The type of plaque you have is also important. Some people have vulnerable or unstable plaque. There's usually a large volume of these types of plaques, narrowing the arteries. As the plaque grows, it affects blood flow," says Elisabeth Kleivhaug Vesterbekkmo.
She is a chief physician at St. Olavs Hospital's Clinic for Cardiology.
"Additionally, plaque usually has a high fat content, and is surrounded by a thin membrane or capsule that can easily burst. It’s like a huge pimple,” she says.
Different types of cholesterol
This process is called atherosclerosis, which means hardening of the arteries. It is caused, among other things, by cholesterol. It's something most of us don't think about much until we reach a certain age. But by then, it may be too late.
The number of people who die from cardiovascular diseases has decreased significantly in Norway over the past 40 years. Nevertheless, over 10,000 people have acute heart attacks every year.
“The question is: Could any of these have been avoided? We know that over 55 per cent of these heart attacks have what we call metabolic drivers. This especially involves high LDL cholesterol as well as elevated blood sugar and high blood pressure,” says Vesterbekkmo.

Researchers agree that there is a direct causal relationship between LDL cholesterol and atherosclerosis. The more LDL cholesterol circulating in the body, the higher the risk of inflammation and plaque buildup.
“Everyone is in agreement about this. There's an overwhelming amount of data confirming it. The lower the LDL, the better the situation,” says Vesterbekkmo.
However, there are also other cholesterol-containing particles that raise the risk of cardiovascular diseass. These are substances that are not routinely measured.
One example is VLDL cholesterol, a type of fatty substance that has a high triglyceride content.
“VLDL cholesterol has been shown to increase plaque formation,” she says.
Another important fatty substance in the blood is lipoprotein(a), commonly called Lp(a). This substance consists of an LDL particle that has a special protein called apolipoprotein A bound to it.
High levels of Lp(a) increase the risk of cardiovascular diseases. Approximately five per cent of the population have significantly elevated levels of this risk factor. It is hereditary.
“If there's a significant history of cardiovascular diseases in the family, patients should be checked for an elevated level of Lp(a),” the researcher says.
The bad guys in your blood
Some people have a heart attack without having elevated levels of LDL cholesterol in their blood.
“This means that we have to look for other causes,” says Vesterbekkmo.
One common factor for all pathogenic cholesterol-containing particles is that they have a small additional protein attached to them, called Apo-B.
“Apo-B is a real bad guy. We can measure Apo-B levels in the blood, which tells us how many circulating Apo-B particles you have that can reach the walls of your blood vessels. This gives us important additional information,” she says.
In other words, a person can have what appears to be a perfectly acceptable cholesterol level, when only LDL cholesterol, HDL cholesterol, and the total cholesterol in the blood are measured. This is the standard cholesterol test that you get at your GP’s office.
At the same time, people can have elevated levels of other lipoproteins. This means that you have increased cardiovascular risk without knowing it.
“Cholesterol levels increase with age. That’s why you should keep an eye on your cholesterol as you get older. For example, if you have significantly elevated levels of Lp(a), you can quickly reach a level where preventive medication is recommended,” says Vesterbekkmo.
Searching for new markers
Julie Caroline Sæther has researched biomarkers that can detect fatty plaque and the risk of future heart attacks. She has been searching for new markers that can be detected through a simple blood test.
“Some patients who are hospitalised with a heart attack do not have the common, classic risk factors. They might not even have had any symptoms prior to the heart attack,” says Sæther.
For these patients, a heart attack seems to come out of the blue. The reason may lie in the type of atherosclerosis the unsuspecting patient has. As Vesterbekkmo puts it: Some types of plaque are more unstable than others.
“Lipid-rich plaque, meaning plaque with a high fat content, is more prone to ruptures. The membrane covering the plaque is thinner and bursts more easily,” says Sæther.
If a rupture occurs, the contents enter the bloodstream. This can quickly turn into a clot that completely blocks the blood vessel, leading to an emergency situation. Quick treatment is crucial to minimise damage to the heart muscle and reduce the risk of further complications.
MicroRNA, Lp(a), and small HDL particles
Sæther, Vesterbekkmo, and colleagues are now trying to find markers in the blood that reveal the presence of fatty and unstable plaque that increases the risk of acute events.
“We have used advanced imaging techniques inside the coronary arteries to determine the fat content in the plaque," says Sæther.
They have done this with patients known to have disease-causing plaque.
"In addition, we have measured microRNA and various lipids in the blood to see if we could find markers that indicate the fat content of the plaque,” she says.
The researchers found one microRNA and two lipid particles. These have been shown in other research to be associated with atherosclerosis.

“We found that patients with fatty plaque had higher levels of a microRNA called miR133b. These patients also had higher levels of Lp(a) and free cholesterol in the smallest HDL particles. However, we need more research before we can say with certainty that our findings are correct. We need to carry out larger studies with more patients,” says Sæther.
All the patients in the study were using cholesterol-lowering medications.
“This probably erased some potential findings, but we know that both HDL and Lp(a) are not significantly affected by statins,” she says.
At the same time, research on miR133 and lipid subgroups is divergent. According to Sæther, there is still a lot of lab work that needs to be done.
“Although we now have adequate methods to measure microRNA, the analyses are costly and time-consuming. By contrast, the methods used to measure subgroups of lipids have become so good that using them in clinical practice may be possible if it's seen that they provide important information about risk,” says Sæther.
Checking family history is important
At the Clinic of Cardiology, Vesterbekkmo is focused on the early detection of potential future heart patients as a preventative measure.
“Our aim is to slow down the atherosclerosis process at an early stage. If we identify young people with high cholesterol and start treatment early, we can prevent disease to a large extent,” she says.
If you come from a family where either parent has had heart problems early on in life, you may be genetically predisposed. Early means before the age of 55 for fathers or before the age of 65 for mothers.
Having middle-aged cousins, aunts, and uncles who have had to undergo artery unblocking procedures may be a further sign of genetic predisposition.
“This may be a sign that you may have an elevated risk, which you can actually do something about, but you need to know your lipid profile. In addition, you must take other more traditional risk factors into consideration,” Vesterbekkmo says.
Familial hypercholesterolemia (FH) is one of the most common inherited conditions in the population. Approximately 1 in 200–300 Norwegians have this genetic defect, many without knowing it.
Vesterbekkmo thinks doctors should start with the simplest things: Asking the patient if there is a history of heart disease or strokes caused by atherosclerosis in the family.
“If you combine family history with cholesterol measurements, you quickly get an important overview of risk. However, traditional risk factors must also be taken into account,” she says.
After the fact
Once atherosclerosis is established, the plaque and the disease remain. This is true even if the patient has received treatment with a stent, known as angioplasty. Therefore, both medication and lifestyle changes are important, Vesterbekkmo emphasises.
“Medications can reduce and stabilise plaque to some extent, but lifestyle changes and regular exercise are also important. Our research group has conducted studies showing that regular exercise not only has a positive effect in relation to risk factors, but also affects the plaque directly,” she says.
Exercise makes the plaque more stable, reduces the fat content, and has a beneficial effect on the lipid profile.
However, it does not change the ‘bad’ cholesterol.
“We can't outrun our LDL level. The only way to reduce the level of bad cholesterol is through effective medicines, especially for people with significantly elevated levels. And the sooner, the better,” says Vesterbekkmo.
References:
Sæther et al. Associations between circulating microRNAs and lipid-rich coronary plaques measured with near-infrared spectroscopy, Scientific Reports, 2023. DOI: 10.1038/s41598-023-34642-6
Sæther et al. The association between circulating lipoprotein subfractions and lipid content in coronary atheromatous plaques assessed by near-infrared spectroscopy, IJC Heart & Vasculature, vol. 46, 2023. DOI: 10.1016/j.ijcha.2023.101215
Vesterbekkmo et al. High-intensity interval training induces beneficial effects on coronary atheromatous plaques: a randomized trial. European Journal of Preventive Cardiology, vol. 30, 2022. DOI: 10.1093/eurjpc/zwac309
Vesterbekkmo et al. CENIT (Impact of Cardiac Exercise Training on Lipid Content in Coronary Atheromatous Plaques Evaluated by Near‐Infrared Spectroscopy): A Randomized Trial, Journal of the American Heart Association, vol. 11, 2022. DOI: 10.1161/JAHA.121.024705
———
Read the Norwegian version of this article on forskning.no
More content from NTNU:
-
Researchers are now able to detect aggressive prostate cancer
-
Can desert sand be used to build houses and roads?
-
This is why girls are happiest at school
-
This is what ADHD feels like for an 11-year-old girl
-
Half of all men over 60 have prostate cancer: A new AI tool could help doctors
-
New study: It may become possible to clean boats without toxins





































