An article from Norwegian SciTech News at NTNU

Working to improve the diagnosis of prostate cancer
Severely ill prostate cancer patients are helping researchers test a diagnostic tool that involves injecting a radioactive substance into their bodies.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
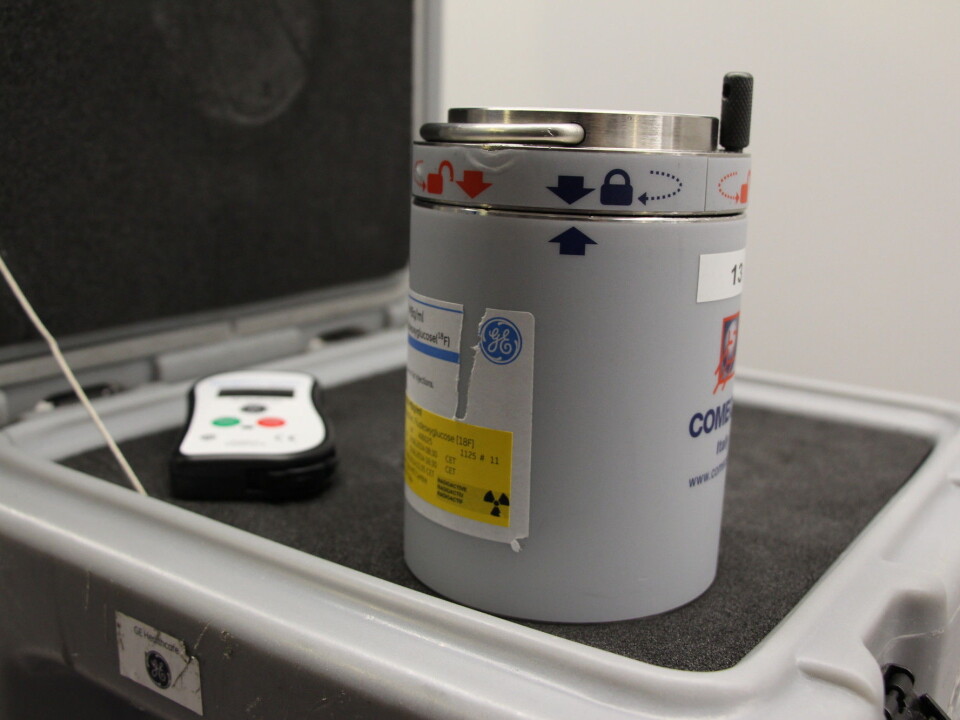
Four doses of a radioactive tracer called 18F- FACBC are on their way from Oslo to Trondheim in a private jet. Three NTNU researchers, one doctor, two radiographers and a bioengineer fidget nervously as they wait. They check the time.
The plane cannot be delayed. Today is a bad day for fog to descend around Oslo’s main airport, Gardermoen, or for there to be a traffic jam between the Trondheim airport and the city hospital, St. Olavs. Everything has to be on time.
Radioactive decay
From the second that 18F- FACBC is injected into its container, it begins to degrade. In 110 minutes, half of the radioactive substance is gone. If the plane is delayed too much, there won’t be any radioactivity left for the last patient. Then more doses have to be flown up from Oslo.
Now the plane is 20 minutes late. Time really is money when it comes to this radioactive substance. One dose costs NOK 30,000. The first patient is already on the table, ready for the procedure. He has an aggressive form of prostate cancer. Doctors fear that it has spread to his lymph nodes.
Now he is waiting to be examined with the most advanced imaging technology that can be found in Norway, a combined PET MRI scan with a price tag of NOK 50 million. He will have to lie still in what boils down to a tiny cave for over an hour while the machine scans and makes images of his blood, bones, and cancer cells.
Finding its way through the body
But this kind of advanced imaging requires a radioactive tracer. With its short half-life, 18F- FACBC (which is an abbreviation for 1-amino-3-fluorine 18-fluorocyclobutane-1-carboxylic acid) has just the right characteristics for the job.
The medical team works quickly when the doses finally arrive at the hospital.
Fortunately, the timing is perfect. First the patient is given an injection of the tracer in his arm, and then placed into the machine, where the tracer finds its way into his veins.
For the radioactive substance to find its way into cancer cells, it needs to have a carrier, a kind of pilot that is able to lead the way to the tumours. In this case, an amino acid acts as the carrier. This is because of cancer cells’ appetite for certain amino acids. A cancer cell is much more active than other cells. It needs more building blocks than other cells, more food. As a result, it attracts and absorbs the amino acid that has been injected into the body.
The radioactive tracer is picked up by detectors that are placed in a ring around the patient in the scanner, and the machine makes images of the cancer cells that light up from the tracer. At the same time, MRI photos of the area are taken, so that doctors get a unique package of information to help them determine which type of treatment is appropriate.
Eight private jets
After an hour, the scan is over and the patient is backed out of the PET MRI. A day later, all of the radioactivity will have left his body. In a few days, he will be in surgery. Hopefully, he has a number of healthy years left to live.
It will take a few years, however, before researchers will be able to conclude how PET MRI scans can be used to improve the diagnosis and treatment of prostate cancer. First, they need to conduct their study with 32 patients. Eight private jets of radioactive tracer will need to be flown to Trondheim, at a cost of NOK 960,000 for this substance.
Shorter, less involved surgery
This is the first research study in the world where amino acids and PET MRI are being used to try to improve the diagnosis of prostate cancer.
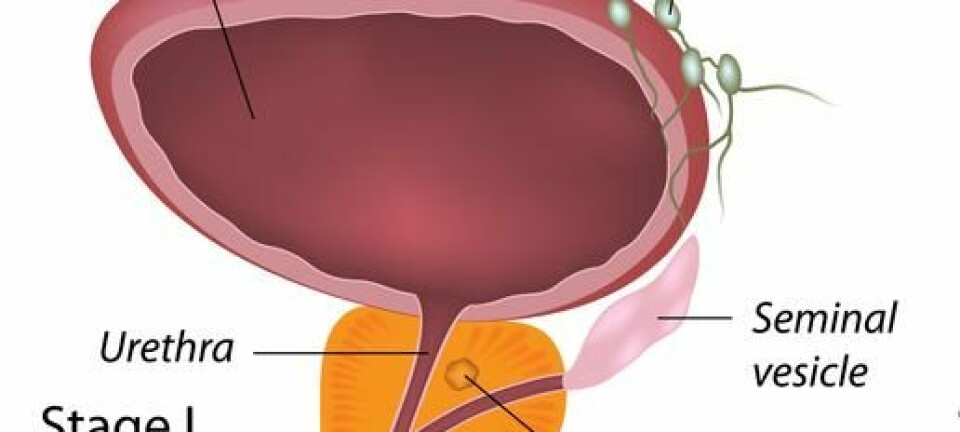
Currently, doctors remove the lymph nodes found in the pelvis of patients with aggressive prostate cancer, without really knowing if it is necessary. Only by cutting into the lymph nodes after they have been removed can doctors determine if the cancer had actually spread.
The NTNU researchers’ goal is for PET MRI to be able to do this detective work before the patient has to undergo surgery, so that surgeons know whether or not removing a patient’s lymph nodes is actually necessary. As a result, some patients should be able to have shorter, less involved surgery, which means less side effects and potential complications.
Diagnoses and the answer key
Researcher will go through the images of all 32 study participants, and then compare these images to their “answer key”, which in this case are the lymph nodes that were removed and biopsied from the patients. Comparing the nodes with the PET MRI images will show whether or not the scans can be used to help in the diagnosis of prostate cancer.
This article is based on interviews with Mattjis Elschot, Elise Sandsmark and Kirsten Margrete Selnæs, all of whom are researchers from the MR Cancer group in NTNU’s Department of Circulation and Medical Imaging. They are working in with Professor Tone Bathen and employees at St Olavs Hospital on the study. Surgeon Eirik Kjøbli of St Olavs Hospital was also interviewed. The study has been financed by the Norwegian Cancer Society.