THIS CONTENT IS BROUGHT TO YOU BY the University of Bergen - read more
Mini-brains may enable new treatments for brain disorders like epilepsy
Using advanced stem cell technology, researchers have developed mini-brains that can mimic brain disorders.
Mitochondria, known as the powerhouses of cells, are crucial for supplying the brain with energy. When this function fails, it can lead to severe brain disorders.
A research team at the University of Bergen has been able to study how genetic mutations in these powerhouses affect brain cells and other cell types, using mini-brains.
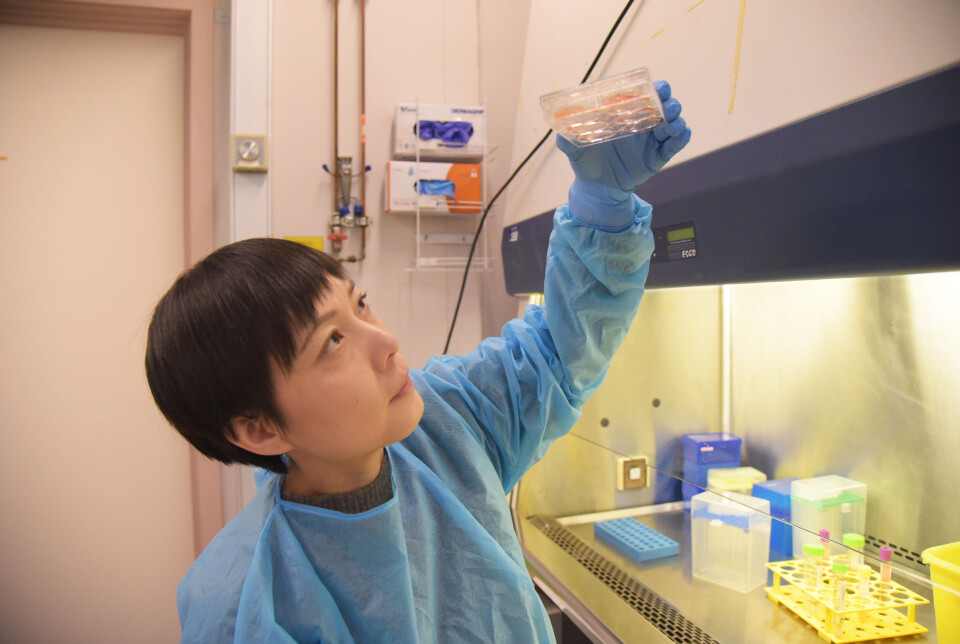
This work is led by Kristina Xiao Liang at the Department of Clinical Medicine.
"The mini-brains give us a unique opportunity to understand disease mechanisms at the cellular level and test potential treatments. This is a significant step towards developing new therapies for diseases like severe epilepsy," says Liang.
Using stem cells
Mitochondrial dysfunction can result from a variety of genetic and environmental factors.
This can affect tissues with high energy demands, like the brain, potentially leading to neurological symptoms, including epilepsy.
Environmental factors such as oxidative stress, toxins, and certain medications, can worsen these symptoms. Oxidative stress is an imbalance between the production and neutralisation of harmful byproducts in cells.
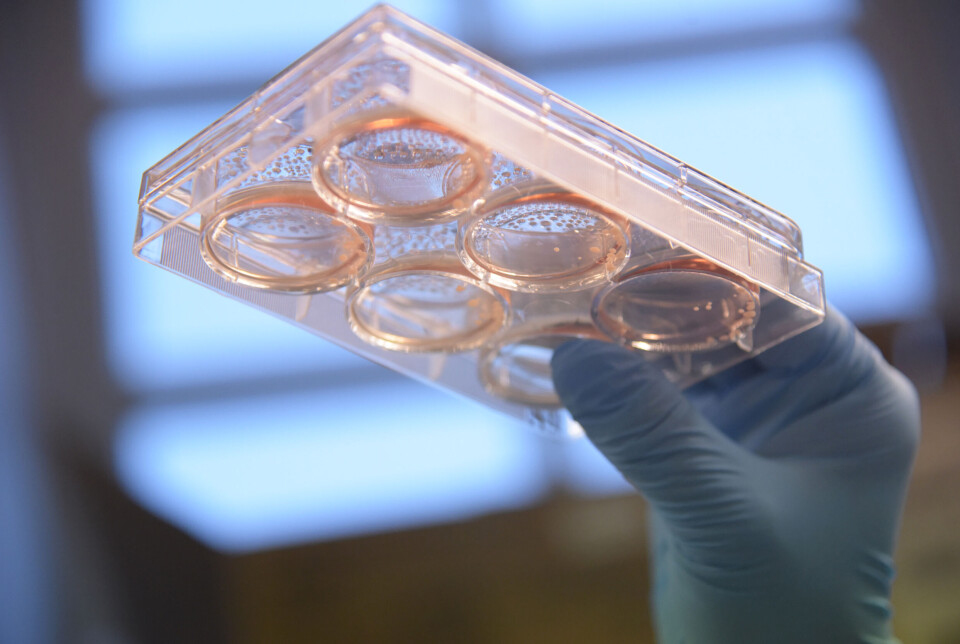
To create the mini-brains, researchers used stem cell technology. Stem cells have the ability to develop into different cell types in the body. They can replace damaged or diseased cells and tissues, helping to repair tissue after injuries or treat diseases that affect cells, such as cancer or diabetes.
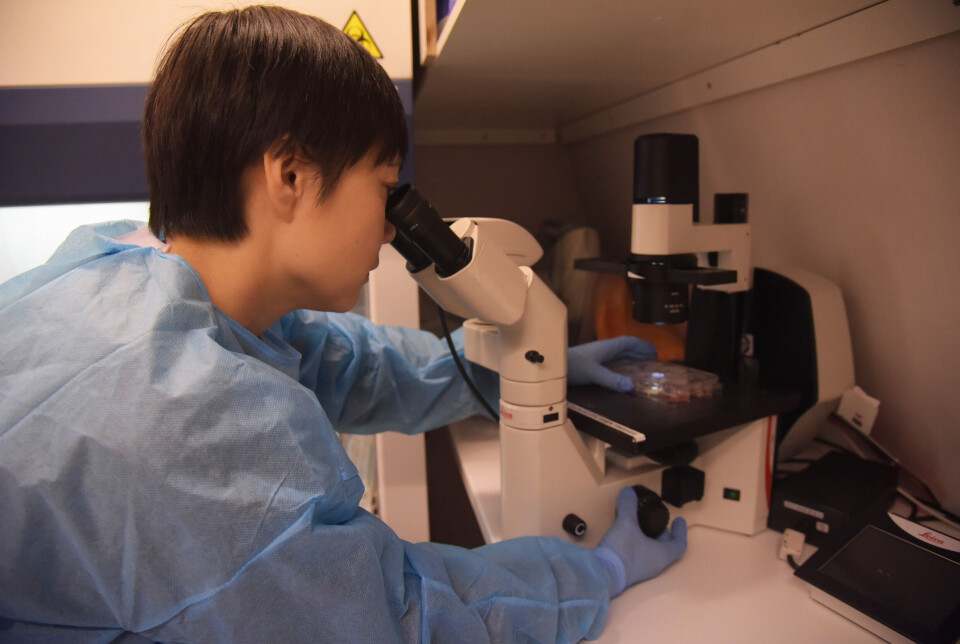
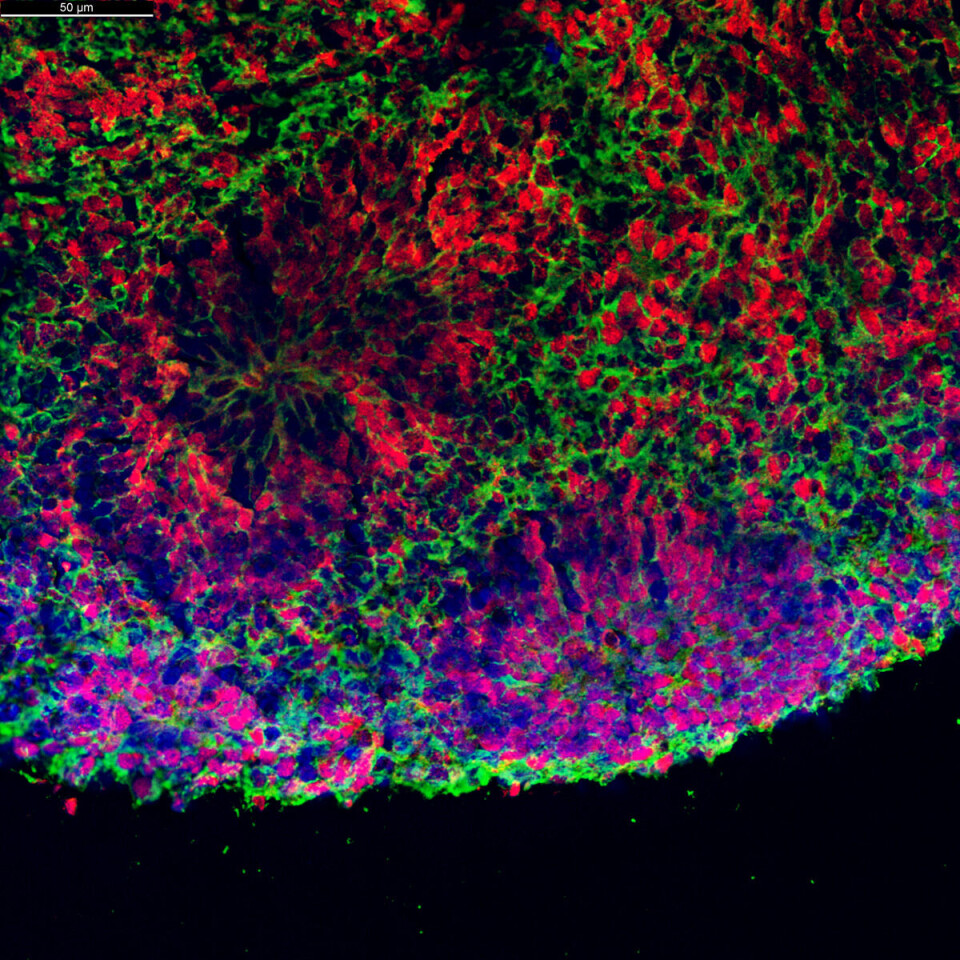
Over time, the mini-brains have organised into structures resembling the developed human brain, including neurons and glial cells. These are specialised cells in the brain and spinal cord that support the main nerve cells in their functions.
The researchers derived the mini-brains from stem cells taken from real patients with mitochondrial diseases.
May be more common than previously thought
Globally, mitochondrial diseases are considered rare, with experts estimating only 1 in 50,000 to 100,000 people affected.
However, there may be undetected cases, according to Kristina Liang.
"The actual number could be higher due to misdiagnosis or underdiagnosis. These disorders can manifest with a wide range of symptoms, from mild to severe, which complicates early detection," she says.
Researchers are now exploring several new treatment methods for patients with such disorders.
These include gene therapy targeting specific DNA mutations, metabolic supplements, and cell-based therapies involving the transplantation of healthy mitochondria or stem cells.
Great potential
The researchers believe the use of mini-brains in research could also be applied to other neurological diseases, such as Parkinson’s and Alzheimer’s.
"These diseases often involve mitochondrial dysfunction that can be studied in the mini-brains. They allow researchers to study disease progression in real time," says Liang.
They can also test personalised therapies and identify new drug targets.
"While they're still under development, they've shown that we can increase our understanding and treatment of these conditions, potentially revolutionising the field," says Liang.
A significant limitation of this research is that mini-brains are not fully matured.
"They resemble the developed human brain, but lack full functional and structural maturity. This may limit their ability to model diseases accurately," says Liang.

Additionally, mini-brains lack the brain's blood supply network, which is essential for studying the blood-brain barrier – the protective 'barrier' between blood vessels and the brain. This barrier prevents harmful substances like bacteria or toxins from entering while allowing crucial substances like oxygen and nutrients to pass through.
Furthermore, using isolated cells in disease modeling may not fully replicate the actual immune response.
"These are challenges we're actively working on to improve our models," says Liang.
Reference:
Chen et al. Hallmark Molecular and Pathological Features of POLG Disease are Recapitulated in Cerebral Organoids, Adv Sci (Weinh), 2024. DOI: 10.1002/advs.202307136

This content is paid for and presented by the University of Bergen
This content is created by the University of Bergen's communication staff, who use this platform to communicate science and share results from research with the public. The University of Bergen is one of more than 80 owners of ScienceNorway.no. Read more here.
More content from the University of Bergen:
-
The proteins in your blood can reveal early signs of heart problems
-
Electricity against depression: This may affect who benefits from the treatment
-
Quantum physics may hold the key to detecting cancer early
-
Researcher: Politicians fuel conflicts, but fail to quell them
-
The West influenced the Marshall Islands: "They ended up creating more inequality"
-
Banned gases reveal the age of water




































