THIS CONTENT IS BROUGHT TO YOU BY University of Oslo - read more
New insight into severe liver disease
There is still much we do not know about primary sclerosing cholangitis. New research provides another piece in the scientific puzzle.
Primary sclerosing cholangitis (PSC) is a severe and chronic liver disease. It affects more men than women, and most people who are diagnosed with PSC are between 30 and 40 years old.
“There is no effective treatment for PSC. The disease is therefore the leading indication for liver transplantation in both Norway and the Nordic countries,” Xiaojun Jiang says.
She is a researcher at the Norwegian PSC Research Center (NoPSC) at the University of Oslo and Oslo University Hospital.
Inflammation causes severe liver damage
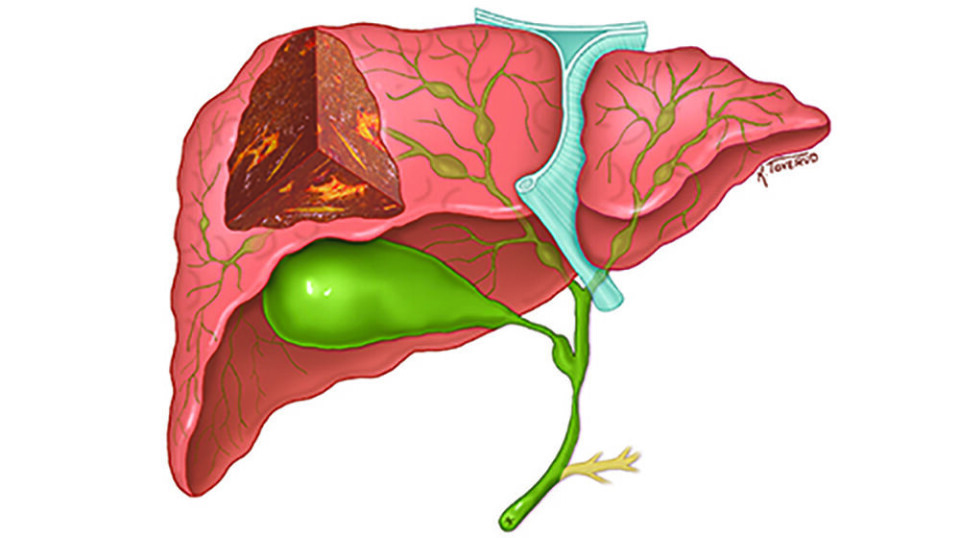
PSC is characterised by inflammation in the bile ducts, which is a system of tubes both in and around the liver.
The bile ducts carry bile from the liver to the small intestine. Bile is an important part of our digestive system and helps to break down and absorb fats from the food we eat.
The inflammation causes scar tissue to form in the bile ducts, making them narrow. This leads to a build-up of bile that gradually causes serious liver damage.
PSC is an autoimmune disease
The cause of PSC is still unclear. The aim of NoPSC is to drive the search for understanding the disease and ultimately finding a cure for PSC patients. The centre has increased the understanding of mechanisms underlying disease development.
What we do know is that PSC is an autoimmune disease, meaning that the immune system, instead of protecting us from infections, attacks and damages cells in the body.
But what makes the immune system attack the body and cause inflammation in the bile ducts?
An interaction between immune cells and cells in the bile ducts
The bile ducts are lined with cells called cholangiocytes. They form the tubes that allow bile to be transported through the biliary system.
In a new study, researchers at NoPSC have discovered that something occurs when these cells in the bile ducts encounter the immune cells in the liver.

“There is an interaction between the cells in the bile ducts and the immune cells that initiates an inflammatory process in the immune cells,” Espen Melum says.
He is a professor at NoPSC and the Research Institute for Internal Medicine.
“For some unknown reason, the immune cells of a person with PSC go to the bile ducts and interact with these cholangiocytes. It's as if they're trying to attack the wall of the tube,” Jiang says.
Thus, the interaction between the different cells causes the immune cells to become pathogenic, meaning they start to harm the body's tissues. This in turn triggers an inflammatory process that develops into liver disease over time.
Can the researchers solve the PSC mystery?
The new discovery, published in Gastroenterology, provides researchers with an important new direction for their further work.
“Now that we know that this interaction between the immune cells and the cholangiocytes is important for the development of PSC, we can focus on that interface further,” Jiang says.
Perhaps this finding is fundamental in solving the mystery that is PSC?
“We believe that if we could block the link between the immune cells and the cholangiocytes, we will be able to resolve the inflammation in the biliary system and hopefully prevent PSC from developing,” she says.
Part of the scientific puzzle
Melum emphasises that despite not translating into clinical practice directly, this study is important in providing a fundamental understanding of PSC.
“Basic research lays the groundwork. Without understanding these types of processes, we won’t be able to develop an effective treatment,” he says.
New discoveries points researchers towards which disease mechanisms are at play, according to Melum.
"By understanding these types of disease mechanisms better, we can potentially find novel therapeutic targets for use in treatment. This study is like a piece in the scientific puzzle," he says.
Genetic mutation in a family with PSC
Researchers at NoPSC have been studying this disease for over 30 years.
In 2021, they found a genetic mutation for PSC in a family where several members have the liver disease.
“We found a mutation that causes PSC, and then we inserted the mutation into mice and saw that they were more prone to liver disease,” Melum explains.
However, as it turns out, not all patients with PSC have this genetic mutation.
Relevance for all PSC patients
This new study is based on the previous findings.
The genetic mutation is expressed in the immune cells in the liver. When the inflammatory process starts in the immune cells, specific pathogenic cells develop, which are common in patients with PSC.
Jiang points out that these findings are well documented.
So even in individuals without the genetic mutation, this interaction can occur and create inflammation in the bile ducts, according to the researcher.
“We believe that this also applies to individuals who do not have the genetic mutation. Because it's the interaction with the cholangiocytes that triggers the development of pathogenic cells commonly found in PSC,” she says.
Jiang adds that their study indicates the research conducted on the family with PSC is relevant for all PSC patients.
A window into the black box
According to Jiang, the researchers at NoPSC describe PSC as a black box, meaning there is so much about the disease that we still do not know.
“However, I feel the mutation we have found is like a window on top of the box. Moreover, this new study uncovers something real that we can see through the window, something that is relevant to the disease. This gives us hope that we will find a cure for the patients,” she says.
Reference:
Jiang et al. Cholangiocytes Modulate Cluster of Differentiation 100 Expression in the Liver and Facilitate Pathogenic T-Helper 17 Cell Differentiation, Gastroenterology, 2023. DOI: 10.1053/j.gastro.2023.11.283

This content is paid for and presented by the University of Oslo
This content is created by the University of Oslo's communication staff, who use this platform to communicate science and share results from research with the public. The University of Oslo is one of more than 80 owners of ScienceNorway.no. Read more here.
More content from the University of Oslo:
-
Mainland Europe’s largest glacier may be halved by 2100
-
AI makes fake news more credible
-
What do our brains learn from surprises?
-
"A photograph is not automatically either true or false. It's a rhetorical device"
-
Queer opera singers: “I was too feminine, too ‘gay.’ I heard that on opera stages in both Asia and Europe”
-
Putin’s dream of the perfect family





































