This article is produced and financed by the University of Oslo - read more
Working hard to find therapy approaches designed to fit your cancer
Norwegian researchers are targeting specific genetic mutations in patients with Acute Meloid Leukemia, and believe this approach will improve survival rates. “We have probably reached a limit in terms of what can be achieved using conventional chemotherapy”, says Dr Yngvar Fløisand.
People come in all different shapes and sizes. These factors change throughout our lives as we grow older, and perhaps when we alter our diets or exercise routines.
This is why I can no longer wear my favorite childhood football shirt that I received for my 10th birthday (as much as I’d love to). It’s also why clothing shops always stock a range of sizes for each of the garments they sell; people are different, so the size and fit of the clothes we wear should be tailored to accommodate our different needs.
In recent years, research has shown that, much like the variety of shapes and sizes seen across humans, cancer also comes in many different forms. In fact, the term ‘cancer’ covers at least two hundred different diseases, each with its own set of gene mutations driving hyperactive cell division and tumor growth.
Consequently, just like our approach to clothing, it makes little sense to adopt a ‘one size fits all’ strategy for cancer treatment. Instead, therapy must be tailored to fit the specific needs of individual cancers.
Not all cancers respond to the same treatments

Unfortunately, our understanding of the biology underlying all different cancer types is still far from complete. Consequently, many cancers are still tackled using a non-personalized approach, whereby every patient receives the same chemotherapy drugs that have been used for many years.
Unsurprisingly, the outcomes of this strategy are rather mixed. For the lucky ones, chemotherapy fits well and they respond positively, but for a substantial number of patients, the standard treatment fails and their cancers remain undeterred. For these patients, new forms of therapy are required that better fit their specific cancers.
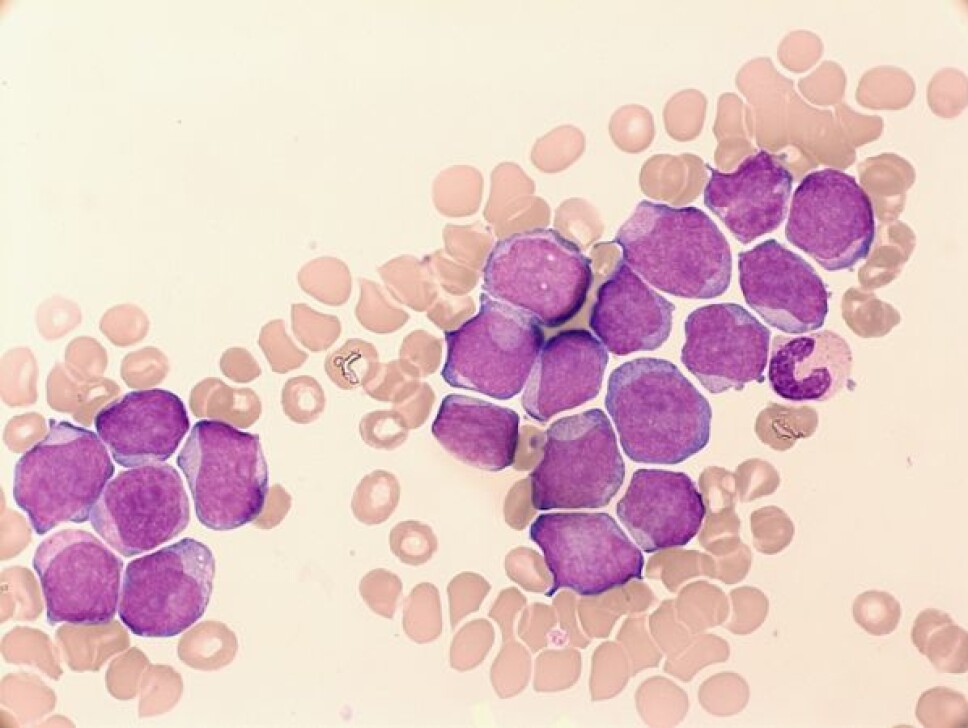
A good example of this involves a type of blood cancer called acute myeloid leukemia (AML). Researchers now know that AML patients can be very different to each other in terms of the gene mutations their cancers possess. In fact, there are several different sub-types of AML, each with a different collection of gene mutations responsible for driving cancer growth.
Despite this variety, the majority of AML patients entering the clinic today still receive the same chemotherapy drugs that have been used in AML treatment regimens for decades. Unsurprisingly, some patients respond better than others.
Finding subcategories to tailor treatment
Dr Yngvar Fløisand is a Head Physician for the AML program at Oslo University Hospital and an associate member of CanCell, a Centre of Excellence hosted at the University of Oslo that works towards reprogramming cancer cells such that they no longer cause disease.
Discussing the problems with current treatments for AML patients, Dr Fløisand says:
“We have probably reached a limit in terms of what can be achieved using conventional chemotherapy. We now need to identify new subgroups of AML patients based on the genetic makeup of their cancers, and then treat these patients with suitable drugs that target the molecules driving tumor growth”.
With this challenge in mind, Dr Fløisand and his colleagues in Oslo have begun to implement a more personalized approach to tackling AML.
When a new patient arrives in the clinic today, doctors take a sample of their tumor and screen the cancerous cells for a range of genetic mutations that are known to occur in some (but not all) AML cases – in other words, to work out which subcategory of AML the patient has.
Subsequently, doctors can tailor the therapy administered to each patient using drugs that are known to be effective against the mutated genes in their cancers.

Targeting genes not just a back-up, it’s the new front-line
One example of a relatively common mutation in AML involves a gene called FLT3.
In healthy individuals, the product of this gene is an enzyme that plays an important role in promoting the growth and development of blood cells. However, in around 25 per cent of AML patients a mutation in FLT3 leads to hyperactive enzyme activity and, consequently, uncontrolled cell proliferation and cancer.
Fortunately, a number of inhibitors exist that are able to block the activity of the FLT3 enzyme, several of which have shown encouraging results in clinical trials involving AML patients. Thus, if screening approaches reveal that an AML patient possesses the FLT3 mutation, FLT3 inhibitors now provide an ideal personalized therapy approach that is designed to fit their tumors.
One such FLT3 inhibitor, named Midostaurin, has been used in clinical trials in Norway, where patients possessing mutated FLT3 who have not responded well to standard therapy have been enrolled on the trials.
After promising results, the decision was made to start including Midostaurin in ‘front-line therapy’ for AML in Norway. This means the drug can be used as soon as a patient is identified as having FLT3-mutated leukemia (not just as a back-up if the standard treatment fails). Doctors hope this transition to personalized AML therapy will have a positive impact on the survival rates for a large number of patients.
Two other genes that are commonly mutated in AML are called IDH1 and IDH2. As the names suggest, these genes are closely related, and play important roles in cell metabolism pathways within cells. Although researchers do not fully understand how mutations in these genes cause leukemia to develop, a significant proportion of AML patients (7-10% for IDH1 and up to 18% for IDH2) posses mutated copies.
As for FLT3, inhibitors exist that can block the activity of the IDH gene products, and as such represent potential opportunities to apply personalized medicine strategies to patients possessing IDH mutations.
Indeed, two compounds called Ivosidenib (blocking IDH1) and Enasidenib (blocking IDH2) have been approved for use in the clinic, and will soon be available as part of front-line therapy for patients in Norway.
Identifying more targets for personalized AML therapy
Clearly, personalized medicine is on the rise, and provides great hope for those patients possessing mutations that can be targeted with drugs in the clinic.
Dr Fløisand predicts the benefits of personalized AML therapy will continue to grow and reach more patients.
“As well as looking for candidate mutations that are already known to promote AML, such as FLT3 and IDH1 and 2, we are also performing non-candidate-based sequencing of the entire DNA genome of patients. As we generate and analyze more and more whole-genome datasets, we will identify more gene mutations that drive AML progression, and better understand how these genes interact with each other”, says Fløisand.
“Ultimately, we will be able to improve our classification of AML subtypes, as well as our ability to assign drugs that can effectively target the mutated genes in each subtypes. At the same time, we are also looking into using compounds with lower levels of overall toxicity, as well as combination therapies, where more than one drug is used to tackle different faulty genes simultaneously”.
Success stories for personalized medicine in Oslo

Dr Åslaug Helland is a researcher at Oslo University Hospital and associate member of CanCell. Her research group focuses on personalized medicine for pancreatic, colorectal and lung cancer, working with patient samples to identify mutated genes that can be targeted with drugs during therapy.
Highlighting the benefit of tailored therapy for these cancers, Dr Helland points to several success stories in Oslo where patients achieved life-changing results following the administration of personalized drugs.
“We have been involved in implementing personalized medicine approaches for many patients who have not responded to standard treatments” says Dr Helland.
“One example involves a lung cancer patient who was diagnosed back in 2011. The patient was a 30 year old male with two children, who described himself as a ‘party smoker’ only. Unfortunately, the cancer was quite advanced and had spread to other organs. The patient began standard chemotherapy immediately, but his cancer did not respond”.
This desperate situation required a new more personalized approach. Dr Helland continues:
“We screened the patient’s cancer for certain mutations, and found one in a gene called ALK. This is a relatively rare mutation in lung cancer, although it is more common in younger patients who are light or never smokers. Fortunately, in 2012, we were able to enroll the patient onto an ‘early access program’ (i.e. prior to formal drug approval) involving an ALK-inhibitor called Crizotinib.”
This had an instant positive effect, much more so than the standard chemotherapy drugs had achieved. Although the effect with Crizotinib was short-lived, the patient subsequently received a range of different ALK inhibitors in the following years, and responded well.
“I’m happy to report the patient is still with us today, working part-time and with a good quality of life. Without switching to the personalized ALK therapy back in 2012, I’m not sure the story would have ended so well” adds Dr Helland.
Still a way to go
Dr Helland hopes this example will soon reflect the way all cancer patients are treated when they enter the clinic, though warns there is a way to go before this hope becomes reality.
“We still lack a comprehensive understanding of the biology underlying cancer progression in different patients. As this knowledge improves, we will be able to identify more potential targets for therapy, as well as more biomarkers that will help us to predict which patients will and will not respond to certain drugs”.
A daunting task, but one that researchers will continue to work on to improve patient outcome. As our ability to ‘measure up’ cancer improves, so will our ability to administer drugs that are exactly the right fit.
———


































