THIS ARTICLE/PRESS RELEASE IS PAID FOR AND PRESENTED BY NTNU Norwegian University of Science and Technology - read more
Ultrasound and bubbles help medicines reach the brain
Combining ultrasound and bubbles helps medicines pass through the protective blood-brain barrier and is giving hope for improved treatment of several diseases.
Luckily, our brain has a filter that protects it and the rest of our central nervous system from foreign elements like pathogens that can damage the tissue.
We call this filter the blood-brain barrier. It consists of proteins that bind the cells in the blood vessel wall, forming an effective physical barrier that is normally absolutely vital.
The filter usually stops 100 per cent of the large molecules and 98 per cent of the small ones found in the bloodstream.
Medicines unable to pass through protective barrier
However, this filter can also present problems when we treat diseases: medication is unable to penetrate the barrier.
“The blood-brain barrier prevents effective treatment of many brain diseases,” says Catharina de Lange Davies, a professor at NTNU’s Department of Physics.
Of the 7,000 drugs consisting of small molecules, only 5 per cent are designed for the central nervous system. Few of them are particularly effective. This is largely due to the blood-brain barrier.
For example, the filter can stop the cytotoxic drugs needed by people with brain tumours, as well as drugs for diseases like Alzheimer’s or Parkinson’s.
Ultrasound and bubbles trick the filter
One solution that several researchers are working on is to inject microbubbles into the blood and treat the brain with focused ultrasound.
Ultrasound causes the bubbles in the blood vessels of the brain to vibrate. This creates mechanical forces that act on the blood vessel wall and open the blood-brain barrier.
Researchers at NTNU’s Department of Physics, collaborating with the EXACT Therapeutics company, have used a completely new type of gas bubble that is larger than the gas bubbles used previously. This technique is called “Acoustic Cluster Therapy,” or ACT.
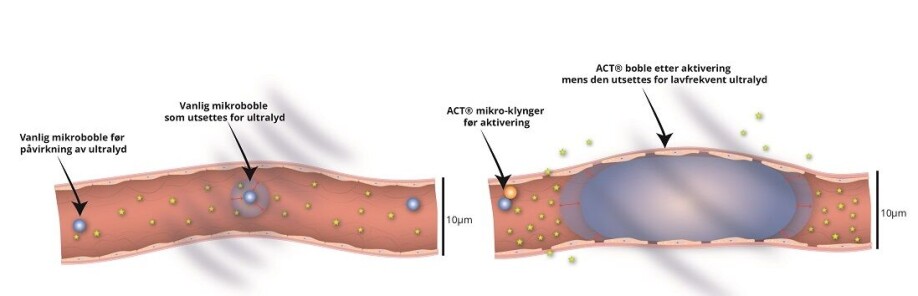
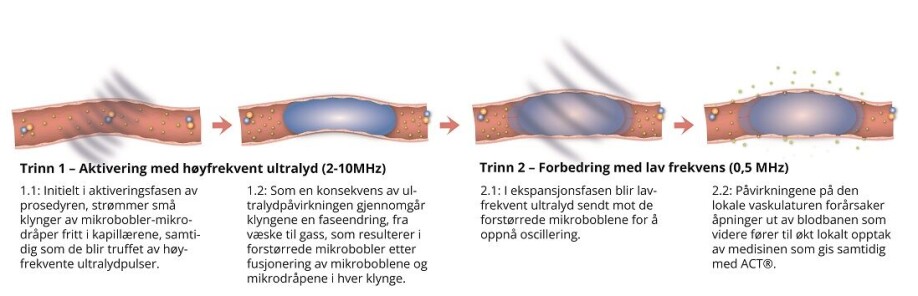
- Small clusters consist of a negatively charged microbubble that attaches to a positively charged drop of oil. These are injected into the bloodstream.
- Ultrasound is then directed at the brain. This causes the microbubble to vibrate and transfer energy to the oil droplet, which then together merge into a single, enlarged microbubble with 1 000 times greater volume than other commercial ultrasonic microbubbles.
- The large size of the microbubble brings it in contact with many of the cells that form the blood-brain barrier along the blood vessel wall in the capillaries. A new set of ultrasonic pulses causes the large gas bubble to vibrate and effectively open the blood-brain barrier.
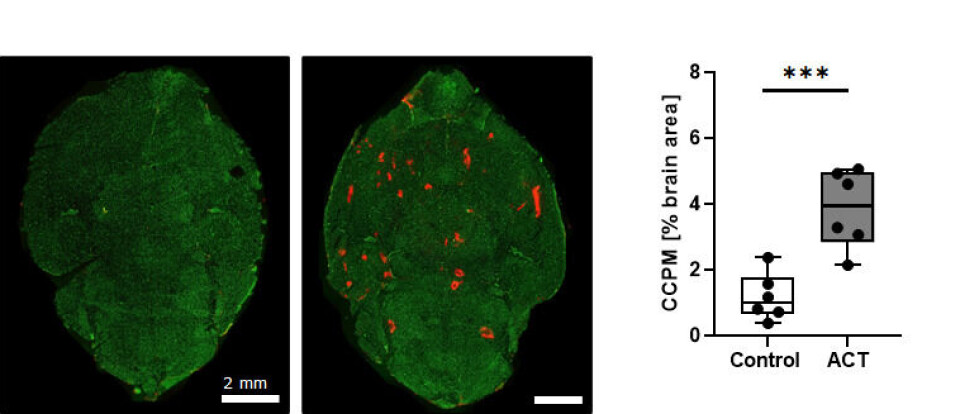
At the same time, medicine – such as drugs encapsulated in nanoparticles – can be injected. Researchers at NTNU have shown that these nanoparticles can cross the blood-brain barrier and reach the brain tissue in mice when using ACT.
The results are very promising and safe.
Medication gets through
“The method increases the permeability of the blood-brain barrier. It also increases the uptake of large molecules and nanoparticles in the brain,” says de Lange Davies. “In our mouse experiments, we’ve shown that the blood-brain barrier closes after about one day, and we haven’t found any significant damage to the brain tissue.
Ultrasound in combination with microbubbles is currently the only method to penetrate the blood-brain barrier in a way that only affects conditions locally and that does not destroy the tissue.
Using the method on patients with brain cancer
“This is a big step towards better treatment for various brain diseases,” says de Lange Davies.
Testing is now taking place on patients with brain cancer and Alzheimer’s in other countries. Ultrasound is used in combination with smaller gas bubbles that are created as a contrast agent for ultrasound imaging. These studies show no side effects from the treatment.
“We think these results are exciting and encouraging. Now we’d like to study the ACT technology in patients with malignant brain cancer,” says de Lange Davies.
Reference:
Marieke Olsman et.al. Acoustic Cluster Therapy (ACT®) enhances accumulation of polymeric micelles in the murine brain. Journal of Controlled Release, 2021.
———
Read the Norwegian version of this article at forskning.no
Read more content from NTNU:
-
This determines whether your income level rises or falls
-
Why is nothing being done about the destruction of nature?“We hand over the data, but then it stops there"
-
Researchers now know more about why quick clay is so unstable
-
Many mothers do not show up for postnatal check-ups
-
This woman's grave from the Viking Age excites archaeologists
-
The EU recommended a new method for making smoked salmon. But what did Norwegians think about this?





































