An article from University of Oslo
Transplantation - a risky treatment
Stem cells taken from bone marrow can save lives, but can also have fatal side effects.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Chemotherapy of leukaemia patients does not only kill the cancer cells, but also healthy, blood-forming cells. Often the patient will need new blood-forming cells.
These can be obtained from the patient's own bone marrow - autologous transplantation - or from the bone marrow of a healthy donor - allogenic transplantation.
The bad news is that allogenic stem cell transplantation is a highly risky operation for the recipient. Five years after transplantation, only half of transplant patients survive.
How the risk of this vital operatin can be minimised is the research focus for Professor of immunology Bent Rolstad and his research group of the Institute of Basic Medical Sciences at the University of Oslo. The group has recently been granted funds from the EU's seventh framework programme.
Growing number of transplantations

Around 20,000-30,000 transplantations of blood-forming stem cells from a donor are carried out around the world each year, and the number is growing.
The human race is living longer, and certain forms of leukaemia tend to afflict people over 60 years old. The patient group which may need a stem cell transplant is therefore still growing.
Leukaemia is the main disease treated using stem cell transplantation, but there are also other forms of cancer and hereditary defects in the immune defence system which account for some transplantations.
Fatal immune cells
One reason for the high fatality rate amongst transplanted patients is that the disease returns. The transplant can also be rejected by the recipient's body.
But the biggest threat is that immune cells from the donor, which are transferred with the transplant, directly attack the recipient's body. This is an immunological reaction called Graft vs Host reaction, abbreviated to GvH reaction.
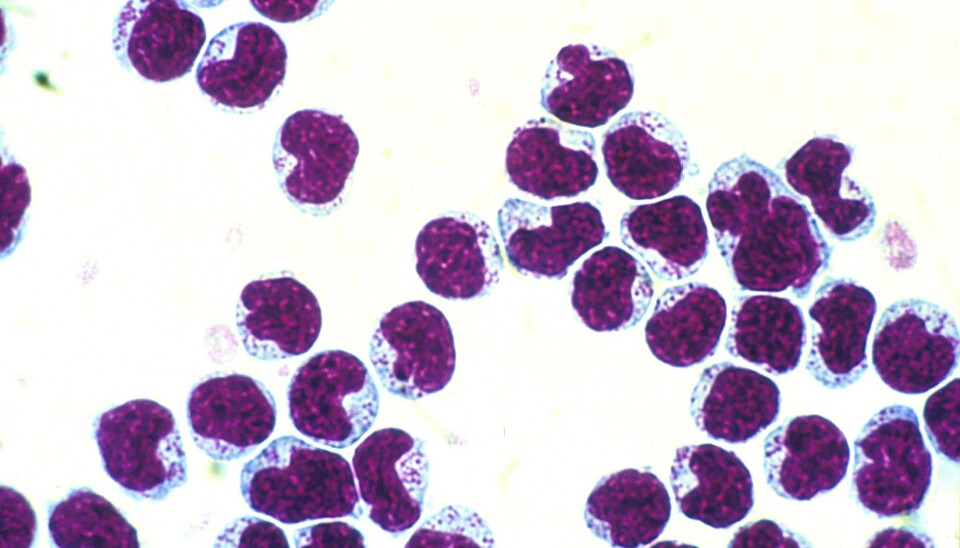
The problem is the T-lymphocytes - white blood cells - which occur naturally in the human body as an important part of our immune defence systems. In the event of a GvH reaction, the T-lymphocytes from the transplant attack and damage the normal, healthy tissue of the host. The transplant host's immune defence system is often weak as a result of cancer treatment, and is therefore unable to combat the aggressive T-lymphocytes from the donor.
"The GvH reaction can cause major side effects, and be difficult to treat," explains Rolstad.
"Many organs can be be hard hit by infections, especially the skin, liver, lungs and membranes in the stomach intestinal canal. Such infections can cause serious invalidity and in the worst case, death," says Rolstad.
Cracking cancer
But the thing about T-lymphocytes is that in the context of stem cell transplantation, they are both beneficial and detrimental at the same time. They can actually trigger a desireable side effect.
As part of their job as immune cells, T-lymphocytes from the donor react to genetic differences between donor and host. Such differences can be expressed in the cancer cells, which triggers the T-lymphocytes to attack them.
The genetic fingerprint
To discover which immune system mechanisms lie behind the two beneficial and detrimental effects of allogenic stem cell transplantation, Rolstad's group are researching genes and cell therapy.
"Based on an animal experiment model which we developed, we are trying to create a sort of genetic fingerprint of both donor and host. We hope this will help us identify which genes in the donor or host can trigger a GvH reaction," says Rolstad.
The model consists of two rat lines, which have exactly the same genes - one line donates the stem cells, the other receives. This allows the researchers to perform systematic studies which are much better controlled than is possible using patient material, when all the patients differ genetically from each other.
"If we find interesting reaction patterns in our study, we can isolate genetic materials from the tissue of the donor and the host, and using a genomic library, we can identify which genes are key to these reactions and what kind of functions they control," explains Rolstad. The genomic library consists of a database of all the rat's DNA sequences.
Through this research, Rolstad hopes it will be possible to select combinations of donor and host which give the least possible degree of GvH reaction, and thus be able to customise each stem cell transplantation to the people involved.
Natural killer cells give the best of both worlds
One of Rolstad's aims is to find treatment combinations which give a doubly-beneficial effect, by halting the GvH reaction whilst triggering the GvL reaction to destroy cancer cells.
This is where cell therapy research comes into the picture. Cell therapy involves introducing cells which can modify the immune defence system's reactions along with the transplant from donor to host. These could for example be regulating immune cells, or primitive stem cells, both of which under certain conditions can suppress reaction to other immune cells.
By utilising the many years of work with the rat model, Rolstad's laboratory has found that part of the answer lies with natural killer cells, or NK cells. In common with T-lymphocytes, these are immune cells which are part of the human immune defence system. NK cells provide the best of both worlds: They can suppress the GvH reaction whilst preventing any leukaemia recurrence by directly attacking cancer cells.
The researchers now want to find the perfect combination of the efficacy of T-cells in a transplant and added NK cells, so that allogen stem cell transplantation will no longer be a risky undertaking.his is called Graft vs Leukaemia reaction, abbreviated to GvL reaction. In this way, allogenic stem cell transplants can destroy any remaining cancer cells in the host.
------------------------
Read the Norwegian verson of this article at forskning.no
































