This article is produced and financed by NTNU Norwegian University of Science and Technology - read more
Cholesterol crystals play an active role in stroke, heart attacks
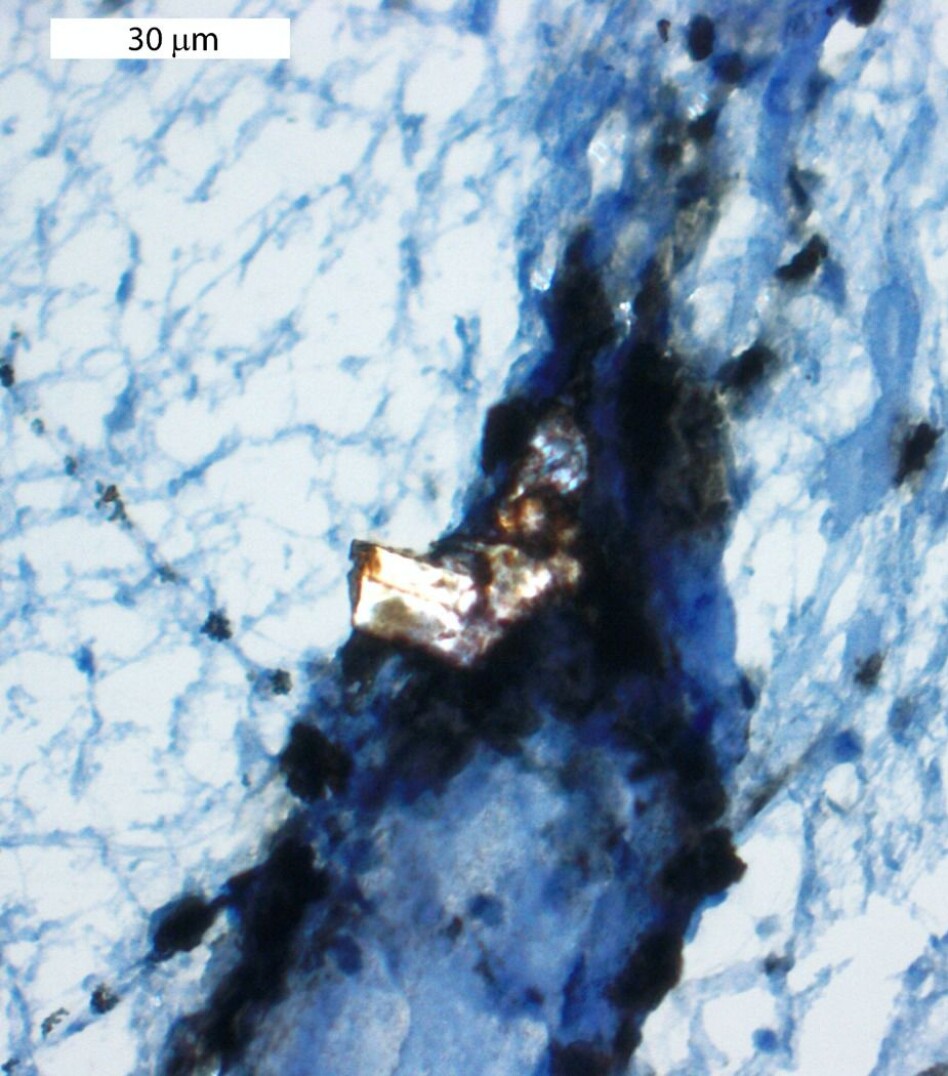
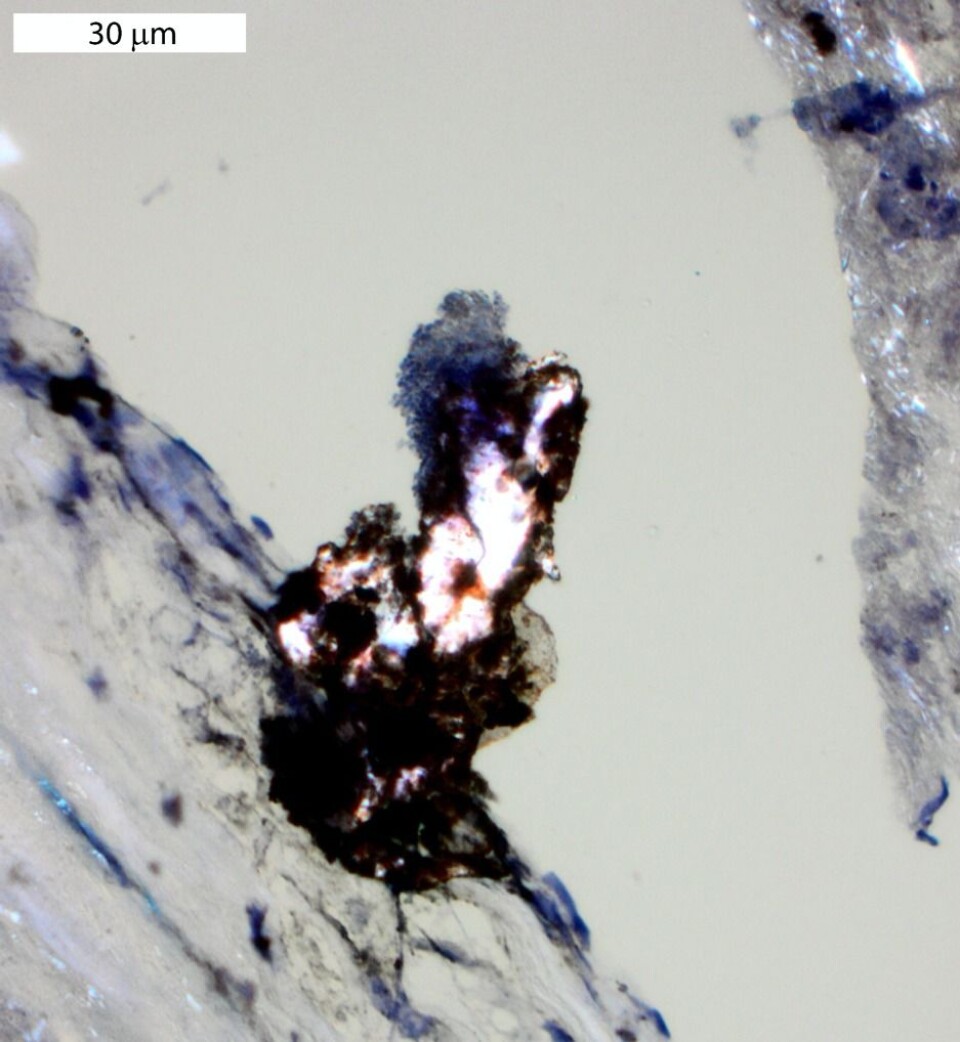
Cholesterol crystals form from “bad” cholesterol and are found in plaques that line blood vessels. When these plaques rupture, they can cause heart attacks or strokes. New research suggests that cholesterol crystals in plaques can actually trigger strokes and heart attacks.
Each and every second of your life, your heart pumps roughly 5 litres of blood through your body. Over the years, and depending on your diet, health and heredity, the vessels that carry blood from your heart can be lined with something called plaques.
A new article from the Norwegian University of Science and Technology’s Centre of Molecular Inflammation Research (CEMIR) suggests that cholesterol crystals found in plaques play a much more active role than previously believed in promoting the blood clots that form after a plaque ruptures.
“Our paper shows for the first time that cholesterol crystals can activate the coagulation system,” said Caroline Gravastrand, a PhD candidate and first author of the article, which was recently published in the Journal of Immunology.
The finding could lead to new intervention strategies to treat cardiovascular disease.
A rupture, then a clot
Cholesterol crystals enter the blood stream when an atherosclerotic plaque ruptures in an artery wall. When this happens, a blood clot typically forms, which obstructs the blood flow to the heart or brain.
Until now, however, researchers didn’t quite know all the details in the series of steps that cause clots to form.
The CEMIR researchers, along with their national and international collaborators, found that one specific immune cell, the monocyte, activates blood clotting by the cholesterol crystals.
Monocytes are an important part of our immune system because they “eat” and destroy harmful material, such as pathogens or dying cells.
Complement system response causes clotting
For the monocytes to recognize cholesterol crystals as harmful material, the crystals have to be marked by defense proteins by a part of the immune system called the complement system. The complement system enhances the ability of antibodies and other cells, like monocytes, to do their job.
“Cholesterol crystals induce monocytes to synthesize and express a protein on the surface called tissue factor – which is responsible for triggering coagulation,” Gravastrand said. “We also showed that this expression is dependent on activated proteins of the complement system.”
CEMIR researchers have previously demonstrated the importance of the complement system in cholesterol crystal induced inflammation.
Blocking complement system stopped clotting
The researchers used a “whole blood” model and also studied blood clots and plaque material from people who had strokes or vulnerable plaques.
When they used inhibitors to block the complement system in blood, the researchers could hinder more than 90 per cent of the clotting that had been induced by the cholesterol crystals and monocytes, said Anne Mari Rokstad, a CEMIR researcher who has led this line of research.
“These findings suggest that prophylactic treatment with a complement inhibitor in patients with advanced atherosclerosis could be a potential new treatment strategy to reduce blood clot formation after a plaque ruptures,” Rokstad said.
“Since one of the complement inhibitors we used is already prescribed to treat a complement-related disease, we hope our data might encourage clinical trials of complement therapeutics in the context of preventing thrombosis (blood clots).”
Other links between vascular disease and inflammation
Rokstad says the research also demonstrates the importance of continuing to study the role of the immune system and inflammation in vascular disease, to understand connections and improve current treatment.
“I believe there are new connections remaining to be explored that are of clinical relevance,” she said.
“We are currently investigating the effects of obesity and diets on the immune system in connection to vascular disease, in a collaboration with Centre of Obesity and Innovation Research at St. Olavs Hospital. We hope our further research will contribute to an increased understanding of vascular disease, also in the context of the obesity epidemic to improve treatment options.”
In addition to the team from NTNU, researchers from the University of Oslo, the Oslo University Hospital, Nordland Hospital/The Arctic University of Norway, the University of Queensland and the University of Pennsylvania contributed.
Reference:
Gravastrand, Caroline S.; Steinkjer, Bjørg; Halvorsen, Bente; Landsem, Anne; Skjelland, Mona; Jacobsen, Eva Astrid; Woodruff, Trent M.; Lambris, John D.; Mollnes, Tom Eirik; Brekke, Ole-Lars; Espevik, Terje; Rokstad, Anne Mari. (2019) Cholesterol Crystals Induce coagulation Activation through Complement-Dependent Expression of Monocytic Tissue Factor. Journal of Immunology. vol. 203 (4).


































