An article from Norwegian University of Life Sciences (NMBU)
Enzyme discovery offers hope of a new generation of antibiotics
Antibiotic resistance is one of our time's gravest threats. New research on cell division offers hope of developing a new generation of antibiotics that can meet the challenge.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
The World Health Organisation (WHO) is among several leading organisations that recently have warned of an increasing threat from antibiotic resistance.
Ultimately, this may result in people dying from what today are considered minor infections.
Expensive to develop new antibiotics
"Very few new antibiotics have been developed in the last 30-40 years because the pharmaceutical industry has had little interest in doing so," says Daniel Straume, a microbiology researcher at the Norwegian University of Life Sciences (NMBU).
He points out that new antibiotics are very expensive to develop, and the earning potential for these types of medicine is too small. But if infections and bacteria-based diseases become resistant to our traditional antibiotics, most of modern medicine will be under threat.
Operations, cancer treatment, transplants and infectious diseases are examples of treatment or diseases where the patient is dependent on antibiotics.
Straume is part of a microbiological research group at NMBU led by Professor Leif Sigve Håvarstein. Together with a research group from Madrid, they have discovered new properties of one of the most important bacteria that cause disease and death in humans. The discovery may contribute to developing new medicine.
The bacterium in question causes Pneumococcal infections and is called Streptococcus pneumoniae. Only tuberculosis bacteria (TB) cause more illness and death than S. penumoniae.
A bacteria that kills
S. pneumoniae is a common cause of morbidity and mortality worldwide, killing one to two million people every year (pneumonia and meningitis), but also cause less serious illnesses such as sinus infections and ear infections, costing the society a lot of money.

Anyone can be affected by pneumococcal infections, but young children and the elderly are most susceptible to be infected and often die from pneumonia.
As a result, the infections are often called 'children’s foe' and 'the old man’s friend'.
Enzyme cleavage
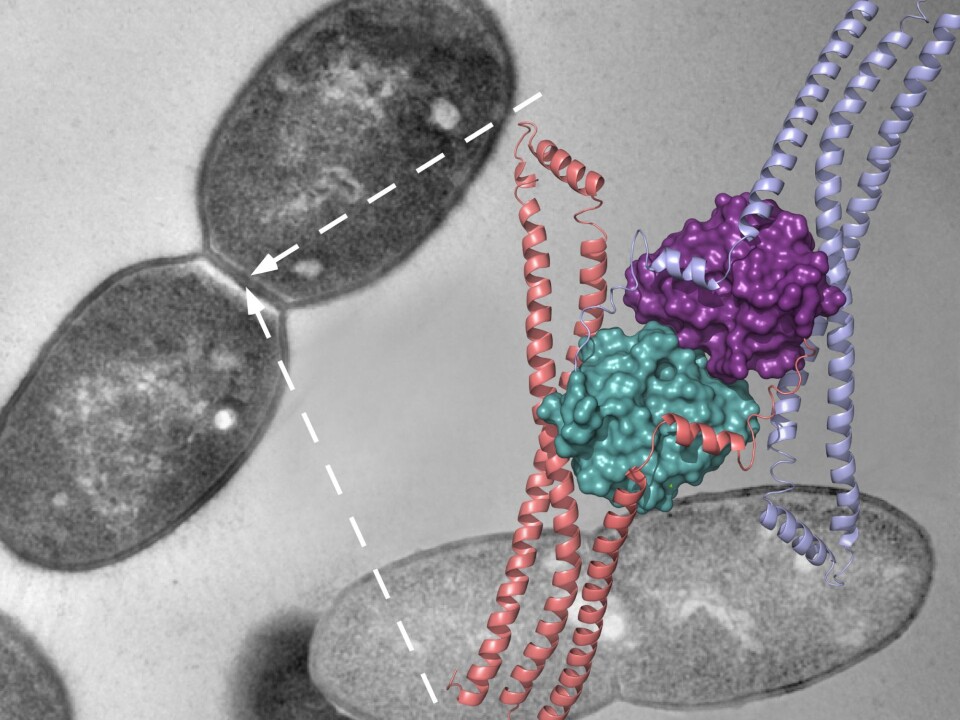
The new enzyme-discovery is related to cell division. This is an absolutely fundamental process where much still remains unknown.
Bacteria usually reproduce by dividing in two. If you have an infection and can inhibit an enzyme that is essential for bacterial cell division, you kill the infection - and the patient recovers.
For a bacterial cell to divide in two, it must construct a cell wall between the two daughter cells.
To complete the division process, this cell wall has to be split in two by being cleaved at the centre.
"What we have discovered is what causes this enzyme cleavage," Straume says.
This means that if this enzyme is inhibited, the disease is stopped.
More resistance
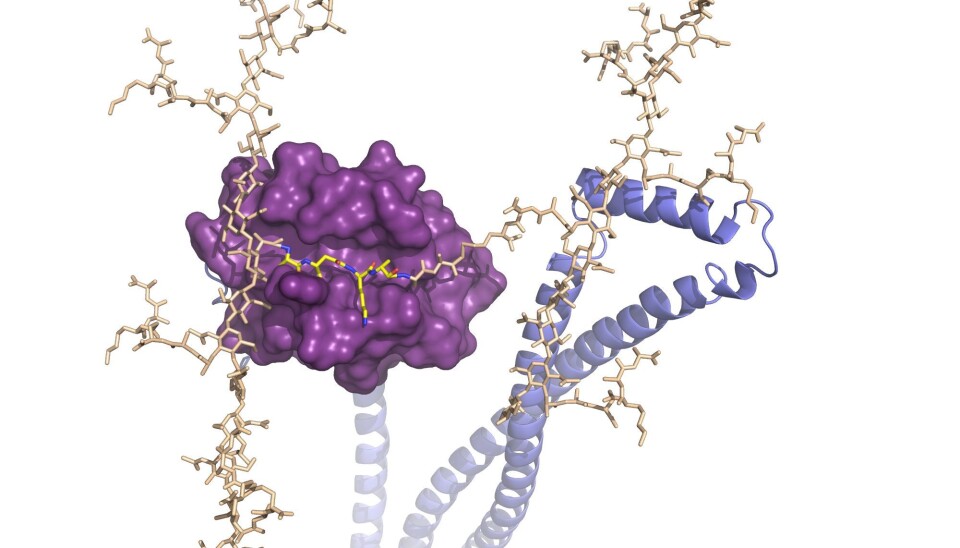
The enzyme is called PcsB and belongs to a group of enzymes called peptidoglycan hydrolases which cleaves the bonds of the cell wall. In addition, the researchers have identified the crystal structure of PcsB.
These findings can, in addition to new insights and understanding of a central biological mechanism, contribute to developing a completely new type of antibiotic.
Pneumococcal infections are treated primarily with penicillin, so-called beta-lactams, that attacks a certain type of enzymes. In the past 20 years we have seen an increasing resistance to beta-lactams and other antibiotics in clinical isolates of S. pneumoniae.
When bacteria are exposed to antibiotics, they will try to change so that they no longer are attacked by the antibiotic. This is what happens when some bacteria become antibiotic resistant.
A race towards new types of antibiotics
What has happened is that the bacteria have been able to modify enzymes inhibited by antibiotics, so that they no longer have the inhibitory effect. Irresponsible and unnecessary use of antibiotics promotes the development of resistant bacteria.
As a result, there is a race between bacteria becoming resistant and scientists being able to develop new types of antibiotics.
"This is not an acute problem in Norway as of yet because we have been more restrictive with the use of antibiotics than many other countries. But in many places in the world this is a problem about to get out of control," says Straume.
He pointed out that cell division is an essential process in the bacterial cell which may be an ideal target for new antibiotics, and PSs is a key enzyme in the cell division process. If one can identify compounds that inhibit the activity of PcsB, these could serve as a new type of antibiotic.
PcsB is also a very suitable candidate for creating a new generation of vaccines against Streptococcus pneumoniae bacteria.
"The fact that we now have the structure of PcsB will be of great help in this work," says Straume.