This article is produced and financed by NTNU Norwegian University of Science and Technology - read more

Norway’s Nobel laureates take up the fight against Alzheimer’s
Developing an effective treatment for Alzheimer’s disease is the long-term goal of a new national research centre in Norway. Nobel laureates Edvard Moser and May-Britt Moser will lead the K. G. Jebsen Centre for Alzheimer’s Disease, aimed at determining how Alzheimer’s disease arises in the brain and its early stages of development.
The Foundation Stiftelsen Kristian Gerhard Jebsen has donated NOK 22.5 million to a national centre for the fight against Alzheimer’s disease. Edvard Moser, from the Kavli Institute for Systems Neuroscience at the Norwegian University of Science and Technology, will lead the new centre, with May-Britt Moser as deputy head. The goal is to translate Nobel Prize-winning brain research from laboratory to patient.
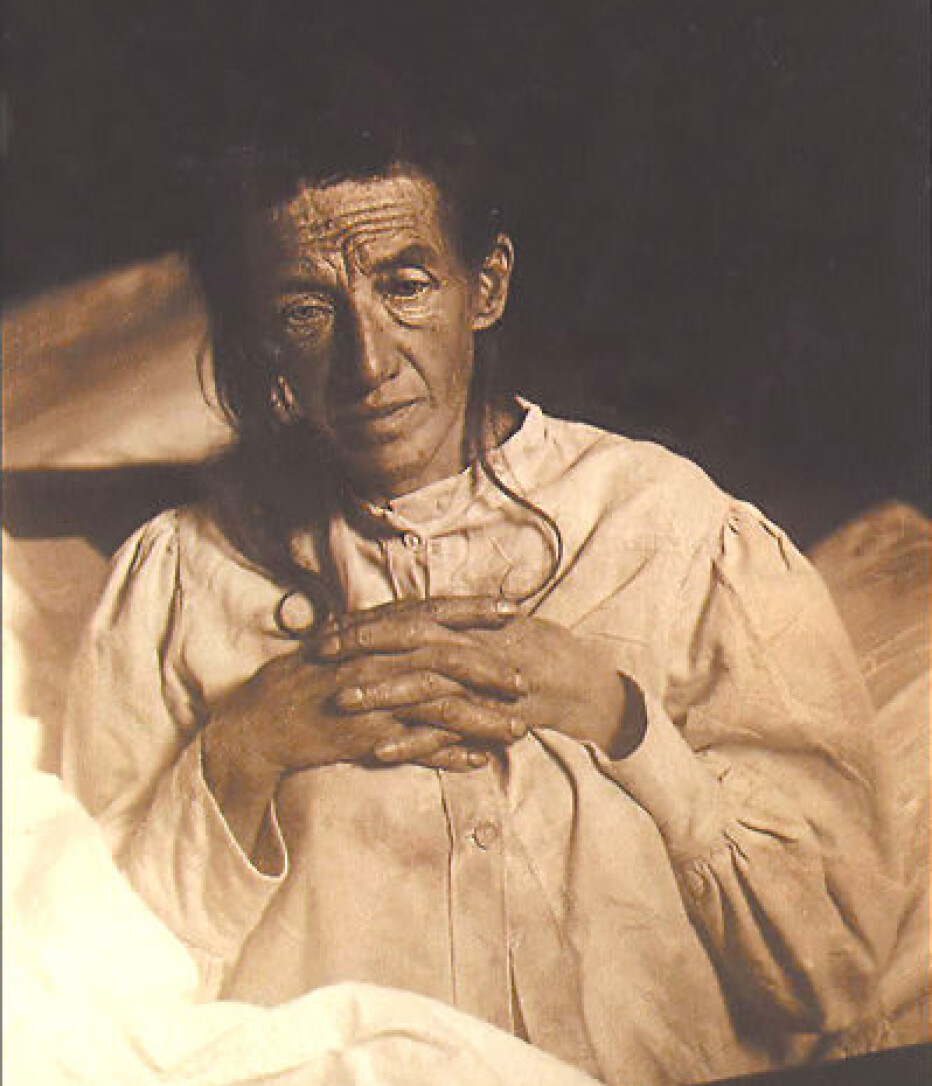
Auguste D and Alzheimer’s diagnosis
The history of Alzheimer’s disease is long and painful. In 1901, a young German psychiatrist meets Mrs. Auguste Deter. Auguste was disoriented, suffering from memory impairment and hallucinations. She had lost much of her language and her husband was no longer able to care for her.
“I’ve lost myself, so to say,” Auguste D. told her psychiatrist. What particularly amazed him was that the woman was in the middle of her life, barely 51 years old and far too young for the disability to be age-related.
Within five years, Auguste was dead. The psychiatrist wondered if her brain held clues that could shed light on the mental illness. With the family’s permission, he examined Auguste’s brain.
Never before had the psychiatrist held in his hands a human brain so severely atrophied. The shrinkage was particularly evident in the cerebral cortex, the outermost layers of the brain where the little grey cells that are so important for higher brain functions reside.
The disease that changes the brain and the mind
To continue his search for signs of the disease, the psychiatrist had to look into the brain. Carefully, he cut the brain into thin slices, which he then coloured with silver salts to increase contrast. Under the microscope he found further traces of disease. Two different forms of accumulation had formed in the cortex of the brain tissue. One type was found in between brain cells, and the other had accumulated inside the brain cells.
Today, these two accumulations are known as beta-amyloid plaques and neurofibrillary tangles of tau protein.
The young psychiatrist was Alois Alzheimer, and the illness he had discovered in Auguste Deter was named after him. Thanks to the Deter family, who gave their consent for Auguste’s brain to be studied, Alzheimer was able to give the world a first glimpse into how this disease alters both the brain and the mind.
Know where the disease starts
Today, more than a hundred years later, Alzheimer’s disease has become one of the greatest threats to public health. The world still knows little about what Alzheimer’s is or what causes the disease, and nothing is known about how it can be stopped. There is no effective treatment.
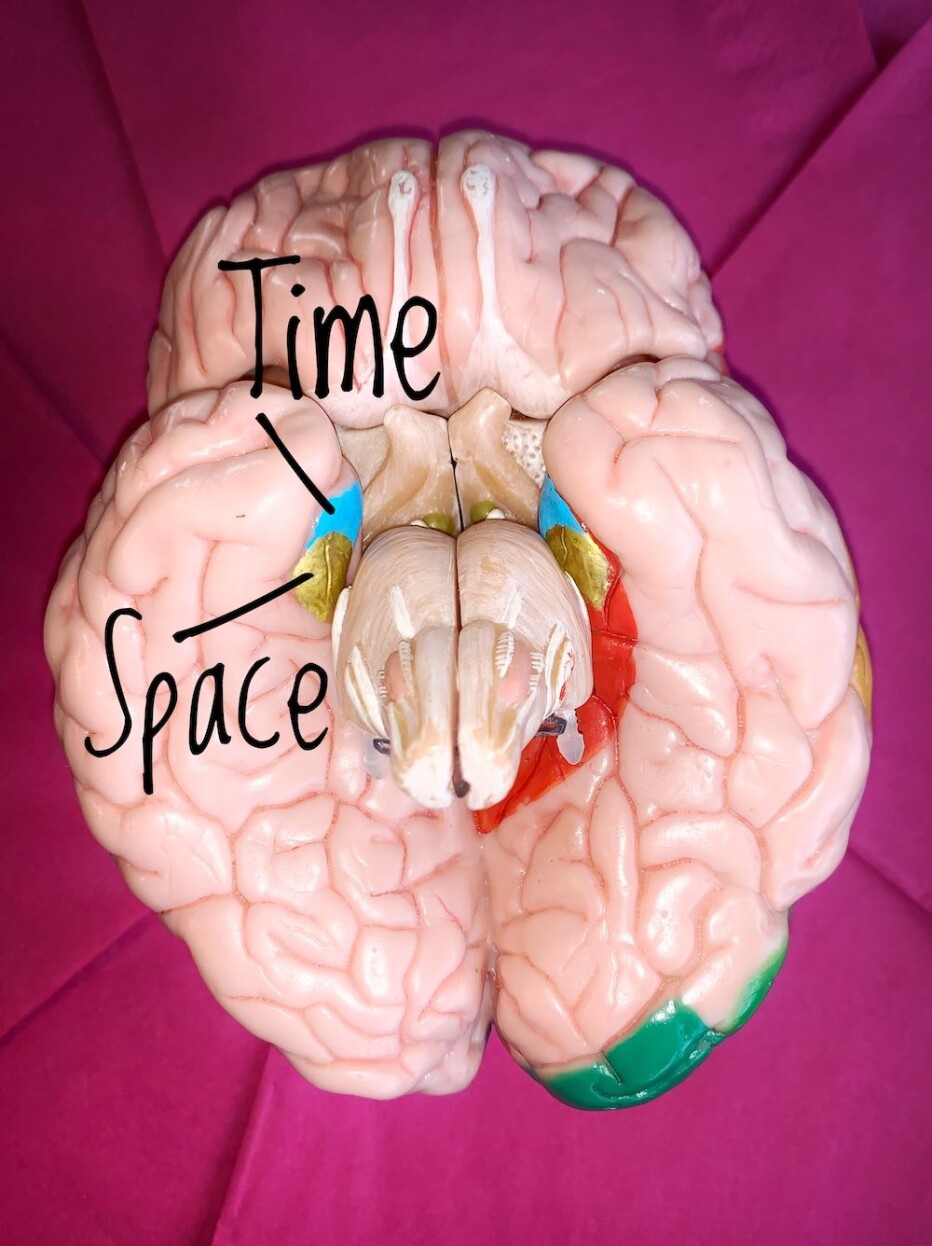
But researchers know where it all starts, deep inside the brain, in an area the size of a fingernail, called the entorhinal cortex. The area is closely interwoven with the brain’s memory centre, which suggested early on that this area had an important function.
Little was known about the entorhinal cortex until 2005, when the Mosers discovered grid cells and found the brain’s seat of space and navigation in the middle part of the brain structure. In 2018, they discovered in the outer end of the entorhinal cortex, a network of brain cells that sort our experiences into the right order, like beads on a string. The sequencing of experiences forms the building blocks of our sense of time.
Cell death starts decades before symptoms are noticeable
The entorhinal cortex gives rise to two brain functions that are fundamental to our ability to make sense of the world: the ability to translate the continuous flow of impressions and events into separate experiences with unique addresses both in space and in time.
It is also the starting point for the massive cell death that works its way through the brain, resulting in the devastating loss of cognitive function that we have come to know as Alzheimer’s disease.
We know that special neurons in the entorhinal cortex are the very first in the cerebral cortex to die from the disease. This cell death starts decades before the earliest symptoms are noticeable.
So it is not surprising that confusion about time and place, getting lost on familiar paths, or having difficulty remembering what you did yesterday or just moments ago are among the earliest symptoms of Alzheimer’s disease.
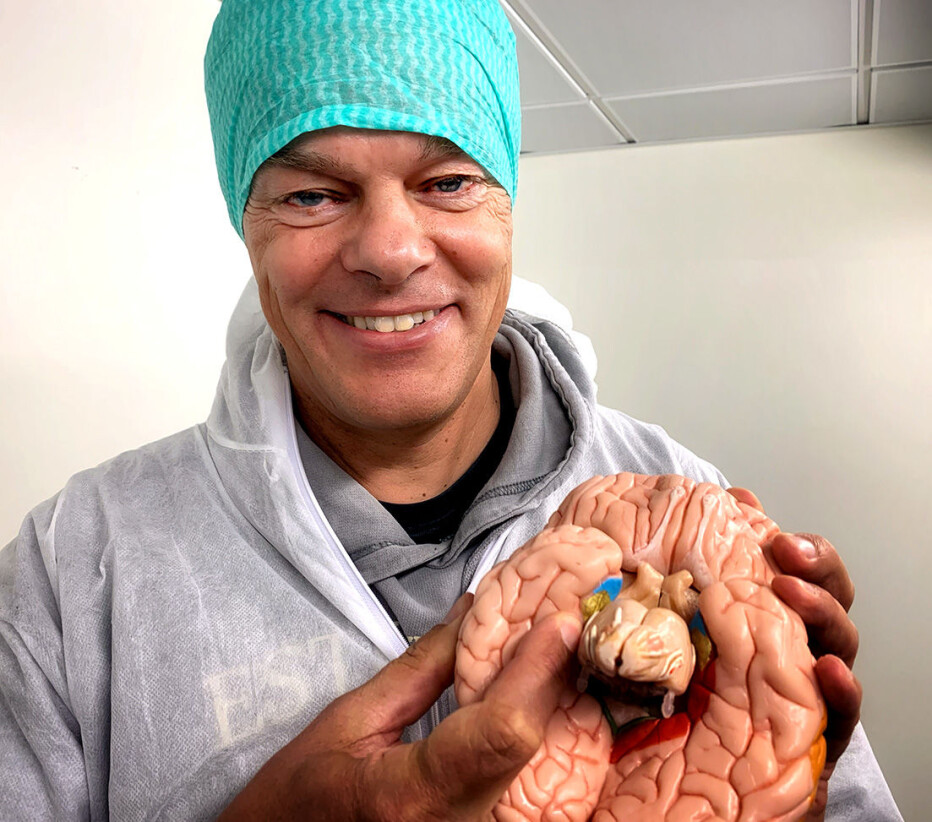
“Our sense of space and time are among the very first brain functions that are impaired in Alzheimer’s,” says Edvard Moser.

Must explore the early mechanisms of the disease
The Jebsen researchers believe there are several reasons why there has been so little progress in the Alzheimer’s field in recent decades.
One reason may be that researchers intervene too late in the course of the disease, when large parts of the brain have already been affected and damaged. Another reason is likely that researchers have conducted their experiments on types of brain cells other than the special entorhinal neurons that are naturally affected by the disease at an early stage.
It is precisely here, in the brain regions where place, time and memory occur, that researchers from the new Jebsen centre will focus their attention.
“If we are to understand what causes Alzheimer’s, we need to identify the early mechanisms of the disease in the particular area where it occurs. We need to uncover reliable biomarkers of the disease which we can use to develop an early diagnosis. Knowledge about the very first route the disease makes may enable us to intervene in the process and stop the disease before cells die and brain functions start to unravel,” says Edvard Moser.
The new centre will bring together Alzheimer’s specialists across disciplines to collaborate on a set of projects designed to bridge the gaps from basic science to clinical implementation. The centre’s research will tackle everything from basic research in rats and mice to clinical research in humans. Each step, from the lab to the patient, will be quality assured with what is called translational research.
Here, promising basic research results on healthy brains will be translated to brains that have been affected by Alzheimer’s disease, and the most significant findings from human brain disease will be translated into animal models for testing before being introduced to humans.
Officially opens 1 October
Edvard Moser and May-Britt Moser will lead the translation of Nobel Prize winning research from bench to bedside. The centre will be located at Øya Campus in Trondheim and will unite university and hospital and link them with prominent national and international partners.
The Jebsen researchers will also have access to state-of-the-art technology. This includes the 7-Tesla brain imaging machine from NORBRAIN 2, which can be used for both basic and clinical research in patients. In the fall of 2019, the MRI machine was hoisted below the ground on the hospital floor (see video).
The K. G. Jebsen Centre for Alzheimer’s Disease will officially open on 1 October 2020, and the money will fund five years of operation.
The national research centre was made possible by a donation from the Foundation Stiftelsen Kristian Gerhard Jebsen of NOK 22.5 million. The Central Norway Regional Health Authority has contributed NOK 11.25 million and NTNU’s Faculty of Medicine and Health Sciences has contributed NOK 5.63 million. The National Association for Public Health, with its expertise and close contact with patients and relatives, will collaborate closely with the centre.
———


































