An article from Norwegian SciTech News at NTNU
Viruses that play hide and seek
Every year, two million children die of acute respiratory infections. Among the culprits are several different viruses, one of which your child almost certainly has had without you or the doctors ever knowing it.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
The good news is that researchers believe you are most likely immune after having had this virus just once.
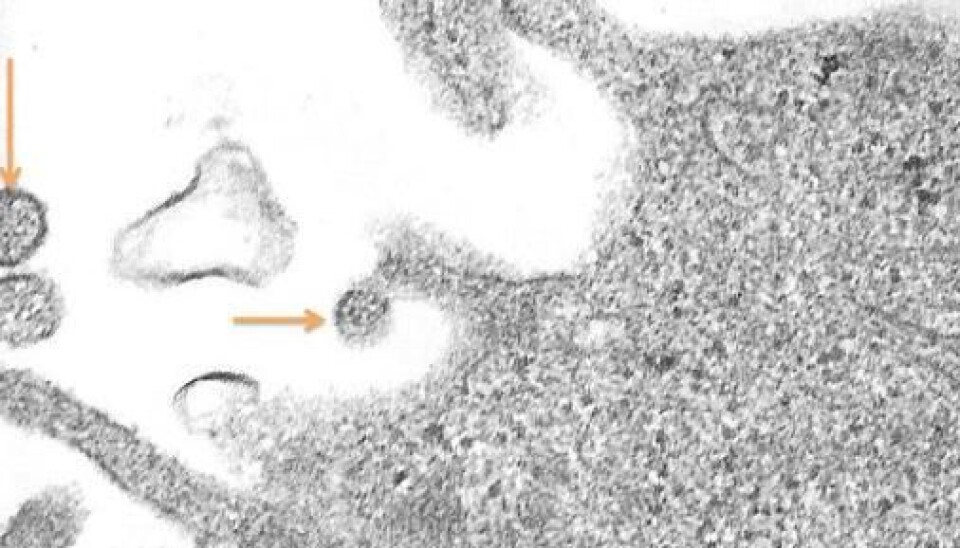
The human metapneumovirus (hMPV) often appears disguised as a cold. Part of the reason it has stayed hidden from doctors is that it was only discovered in 2001. A team of Dutch virus researchers had the thrill of a lifetime when they realized that they had discovered a new virus. Their joy certainly wasn’t lessened by the fact that the virus they discovered turned out to be one of the most common viruses in children who are hospitalized due to respiratory complications.
Can clog the lungs with mucus
According to the World Health Organization (WHO), two million children die annually from acute respiratory infections. Even though the hMPV virus has been able to hide from researchers for a long time, it is not necessarily something you want to experience. Most people will have symptoms similar to a cold, but for some, the virus causes the respiratory system to swell and clog with mucus.
In developing countries, a lot of these children die. In Western countries, infected children are hospitalized and given treatment to help dislodge the mucus and ease breathing. In the hunt for the virus or bacteria that is ravaging a sick child, doctors often find other bacteria. It doesn’t take much to prescribe a course of antibiotics when this happens, just to be on the safe side. The global increase in antibiotic-resistant bacteria is evidence that this process is often unnecessary.

There is just no good way to see if hMPV is the main culprit. At least not yet.
Eager to understand the virus
Ingvild Bjellemo Johnsen, an Outstanding Academic Fellow at the Norwegian University of Science and Technology (NTNU); is working to discover everything she can about hMPV and the body’s response to it. The goal is to understand this interaction well enough to develop new vaccines, good diagnostic tools that allow doctors to more easily find the virus in the body, and new forms of treatment.
This way, more children in developing countries will survive hMPV infections, and the global increase in antibiotic-resistant bacteria may be slowed. These are no small tasks. Luckily, she has been thinking about viruses for the last ten years.
Good at hiding
“I like viruses because they’re smart,” Bjellemo Johnsen says. “They adjust to our cells in a way that benefits them.”
She is most preoccupied with how the immune system is alerted when a virus comes to call. Viruses have one clear goal: to reproduce. To do so successfully, they must be incredibly good at one thing, namely hiding.
On the inside and on the surface of our cells, there are “watchdog” organelles that sniff out viruses and bacteria. They send out warning signals to alert the rest of the immune system about the intruders, which is set into motion attacking the offending virus or bacteria.
Many viruses are able to disrupt or prevent these signals to the point where it results in serious illness and in the worst case, death. This goes for viruses such as Ebola or HIV. Our cells are not able to kill the intruders, so the virus is able to reproduce freely. It is the interaction between viruses and our immune system that Bjellemo Johnsen is trying to understand down to every last detail.
This is what her typical work week looks like:
On Monday, she prepares tests of different types of cells from the human body.
On Tuesday, she turns off a single gene that corresponds to a type of protein in the cells, to see what role this particular protein plays in dealing with viruses.
On Wednesday, she adds a virus and lets it infect the samples for 24 hours.
On Thursday and Friday, she measures the effect of the virus on the samples.
Next week, she does exactly the same thing again. To ensure the quality of each test, she does this three times for each gene and each virus.
Not a blind hunt
“This is how I’m trying to understand the importance of different proteins when this particular virus enters the body. In a few years, I hope to have a lot more answers,” says Bjellemo Johnsen.
There are an estimated 20,000 – 25,000 genes in every cell that can express over 20 million proteins.
“I’m not hunting blindly. We work based on hypotheses about certain proteins being more important than others,” she says. “As a researcher, you have to tolerate answers being negative. You just have to start a new week of work, continue looking.”
Bjellemo Johnsen is a part of a interdisciplinary group of researchers from NTNU and St. Olavs Hospital called CAIR, the Childhood Airway Infections Research Group. The group is comprised of paediatricians, researchers and microbiologists working with airway infections and children.
4000 tests from children with respiratory infections
Asthma is a chronic inflammation. It is the most common cause of hospitalization among children in Norway, a big problem for those it affects, and resource-intensive for society. According to the WHO, 235 million people have asthma globally.
“The reasons that we develop asthma are not very well understood,” Bjellemo Johnsen says. “It looks like there is some kind of relationship between having a serious respiratory infection early in life and developing asthma later. I’d like to look more at this.”
She has access to a solid database of tests from more than 4000 children hospitalized with respiratory infections at St. Olavs Hospital. These tests will be combined with laboratory experiments to uncover potential relationships between respiratory viruses and the development of asthma.