This article is produced and financed by NTNU Norwegian University of Science and Technology - read more

New NTNU method for accurately detecting lung cancer
CT screening to detect lung cancer can save lives. The challenge is to find out who should undergo CT scans. A new method more accurately identifies the right individuals in the risk zone.
The fact that smoking is bad for your health has long been established, and that smoking can lead to lung cancer is likewise well documented. Nine out of ten people who get lung cancer are either smokers or ex-smokers.
However, only a small percentage of smokers actually develop lung cancer during their lifetime. Several studies have looked at how individuals at risk of developing cancer can be detected as early as possible so that they can receive curative care.
Results from the American National Lung Screening Trial (NLST) conducted by the National Cancer Institute in the US and a Belgian-Dutch study (NELSON) show that computed tomography (CT) screening of smokers' lungs saves lives.
Up to two-thirds of at-risk patients go undetected
The problem is that the coarse criteria used to select the participants in these studies involuntarily excluded up to two-thirds of those who later developed lung cancer.
The criteria also included high numbers of individuals who were believed to have lung cancer based on the CT scan but turned out not to, so-called false positives.
Such inadequate selection criteria lead to three clear disadvantages:
CT scans of many healthy individuals may reveal changes that are believed to be cancerous and that lead to unnecessary interventions involving a certain amount of risk and worry.
CT scans should not be conducted unnecessarily since repeated small x-ray doses can be harmful over time.
CT scans are expensive and resource intensive, so it is important to come up with good methods that identify those who actually belong to the small at-risk percentage of individuals as accurately as possible.
This is exactly what NTNU researchers from the Norwegian University of Sciene and Technology (NTNU) have done.
“Our method can reduce the number of people who are subjected to unnecessary CT scans in future lung cancer screenings, and at the same time the method ensures that individuals with the highest risk are identified,” says NTNU Professor Oluf Dimitri Røe.
Created HUNT calculator to compute risk of lung cancer
An international research group with members from NTNU and the University of Crete, led by Røe, has developed a tool for accurately calculating lung cancer risk.
The calculator was developed with data from the Trøndelag Health Study, HUNT, which is one of the world's largest health databases.
The HUNT Lung Cancer Model Risk Calculator calculates your level of risk for developing lung cancer six and sixteen years into the future. You can log in to the calculator to find your personal risk.
The results for this calculator were confirmed in a large population outside the HUNT2 study from several locations in Norway and showed great accuracy.
The HUNT calculator is based on seven factors:
- Age (risk increases with age)
- Smoking pack years (converted into how many years you have smoked 20 cigarettes daily; risk increases the higher the number)
- How many cigarettes you have smoked daily (a few cigarettes daily for many years is more harmful than many cigarettes for a few years)
- How long it has been since you quit smoking (risk decreases with the number of years)
- Body mass index (BMI; the lower the BMI the higher the risk)
- Periods of daily coughing throughout the year (increases risk)
- How many hours you are exposed to indoor smoke daily (risk increases with the number of hours)
Wanted to test a hypothesis
The research group from NTNU and the University of Crete subsequently collaborated with Danish researchers who were conducting the Danish lung cancer screening trial (DLCST), which had a ten-year follow-up period. The researchers wanted to test the HUNT calculator on a population that had already been screened and had follow-ups.
The Danish study compared annual CT screening for lung cancer with no screening in 4104 smokers and former smokers between the ages of 50 and 70. One of the goals was to evaluate whether annual CT screening could reduce lung cancer mortality by more than 20 per cent.

The study followed the test subjects from 2004 to 2015. The criteria for those who participated in the study were: at least 20 pack years, less than ten years since quitting smoking and 50-70 years of age.
The hypothesis was that the HUNT calculator would work better than the criteria used by the recognized NLST and NELSON studies (presented at the beginning of the article) to identify who warranted a lung cancer screening.
A "reduced" HUNT model was created to accommodate the fact that the DLCST had tracked only five of the seven variables used by the HUNT calculator.
The researchers from NTNU and Crete used the same statistical methodology as the original HUNT calculator, but based only on the first five criteria (age, pack years, number of smokes per day, body mass index (BMI) and quitting date).
The HUNT model was then tested on the Danish screening trial to see if it fared better than the NLST and NELSON criteria for predicting who would develop lung cancer.
HUNT model identifies correct cases
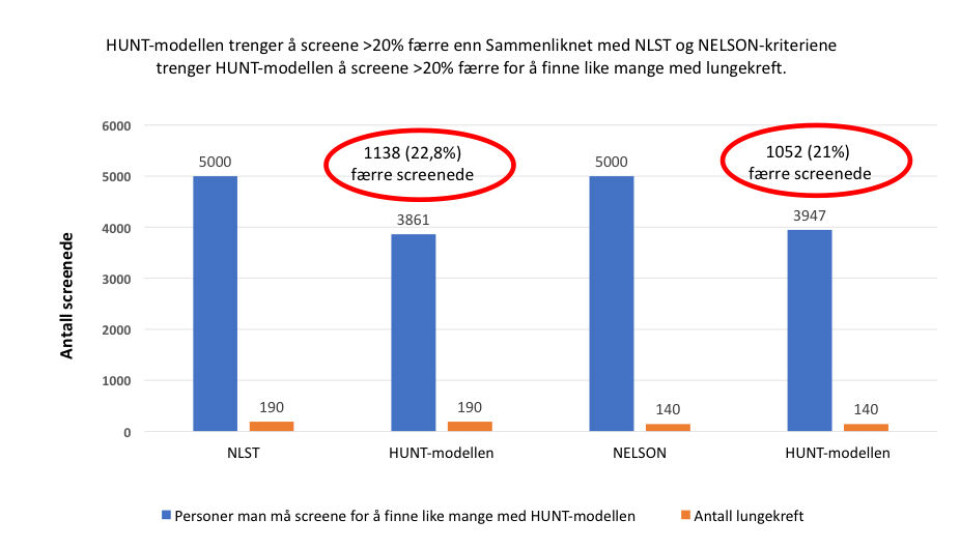
The results showed the HUNT model to be better in all the comparisons. The model predicted 99 per cent of the cases correctly against 70 per cent and 95 percent using the NLST and NELSON criteria, respectively.
In addition, significantly fewer people had to be screened with the HUNT model than either of the other study criteria.
Instead of screening 5000 people using the NLST and NELSON criteria, the HUNT model required screening just under 4000 people, a reduction of more than 20 per cent.
“With the NLST and NELSON criteria, we know that they exclude many high-risk individuals and include a lot of low-risk patients, which is unfortunate and resource intensive,” says Røe.
The HUNT model allows you to determine in advance what risk threshold you can accept for screening, which may vary between countries with differing levels of health service resources. You can choose the threshold that society thinks is the most cost-effective.
Also captures younger at-risk individuals
The study concluded that the HUNT model is superior to both the NLST and NELSON criteria in predicting lung cancer in a high-risk population.
“What’s special about this way of selecting risk in relation to the other criteria is that the HUNT model ranks individuals according to their personal risk, says Oluf Dimitri Røe.
“Our original HUNT Lung Cancer Model Risk Calculator is also able to identify high risk in young people (under 50) and non-smokers, which is not captured by the NLST or NELSON criteria,” Røe says.
Both NTNU studies show that the selection process for lung cancer screening leaves room for significant improvement.
Røe stresses that the key to developing these models has been the fantastic HUNT database.
The database contains data from a large number of people, who have each answered many questions and had a long follow-up period.
“That’s why we’ve been able to use advanced methods in statistics and machine learning to arrive at these data-driven, multivariable predictive models. Our models outperform commonly used criteria that are based only on a person’s age and smoking history,” says Røe.
“We believe that the HUNT models should be included in future screening studies and programmes, especially in Norway where they’ve been developed, but also internationally since they appear to be better, simpler and more accurate than other comparable models.
Reference:
Røe OD, Markaki M, Tsamardinos I, et al. ‘Reduced’ HUNT model outperforms NLST and NELSON study criteria in predicting lung cancer in the Danish screening trial. BMJ Open Resp Res 2019;6:e000512. doi:10.1136/ bmjresp-2019-000512
———