An article from Norwegian SciTech News at SINTEF
Killing cancer cells with super glue
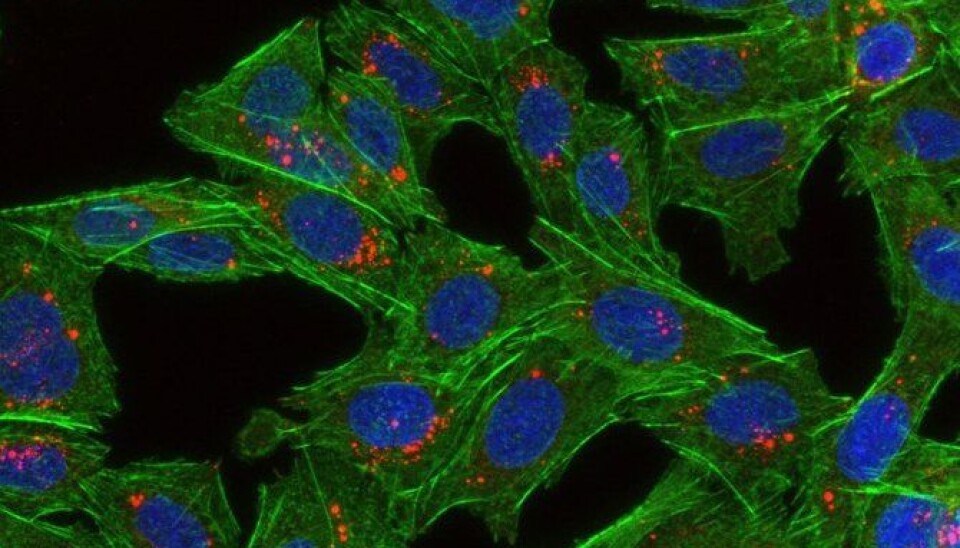
Using nanocapsules made with super glue, researchers have succeeded in making drugs attack tumours with surgical precision.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Researchers have developed a new nanocapsule that exploits the tumour's Achilles heel – poor quality blood vessels, which develop as a result of the tumours rapid growth.
“This makes it easier for us to penetrate the vessels and deliver the cancer drugs directly into the tumour”, says nanomedicine specialist Ýrr Mørch at the Norwegian research organisation SINTEF.
The nanocapsules are transported in the bloodstream with the help of gas bubbles, and secrete the cancer drug when they arrive at the targeted tumour.
They intend to use ultrasound to burst the bubbles when the drug reaches the tumour.

"Ultrasound generates a minute pressure wave and increases the tissue temperature. This makes it easier for the nanoparticles to penetrate the blood vessels in the tumour, where they then disintegrate, release their cytotoxins, and kill the cancer cells," explains Mørch.
“Since the gas bubbles also act as a contrast medium, we can use ultrasound to actually observe the drug treatment in action,” she adds.
A further benefit of this method is that the drug can be made to recognise the tumour.
More potent and fewer side-effects
Studies show that localised drug delivery means that tumours are exposed to much higher doses than is the case with traditional cytotoxin treatments.
Under existing treatments, less than 0.1 percent of the drug actually reaches the tumour. The rest ends up in the liver, kidneys and other organs, which makes the drug of little use and often leads to side-effects.
“When we use targeted treatments, between 5 and 6 percent of the drug reaches the tumour, which greatly reduces its harmful effects,” says Mørch.
“This will allow us to administer lower levels of drugs to patients.”
The researcher’s objective is to achieve a 10 percent effect using the targeted treatment approach.
Making the capsules
One of the challenges the researchers are working on, is how to camouflage the capsules to prevent the patient's immune system from attacking and destroying the capsules before they reach their targets.
This is achieved by manufacturing the capsules in such a way that the body perceives them as droplets of water.
The camouflage is made up of a thin layer of long polymers which attract water and form a small water cloud around each capsule.
"This delays the body's ability to identify the particles, and buys us the time we need to deliver them to the tumour," Mørch says.
The glue is gradually broken down in the body and the drug released.
“In simple terms, we make nanodroplets of glue which are then mixed with the drug,” she says.
The same adhesive is used to bound wounds.
Hope for brain disease treatments
Much of the research is taken up with investigating what happens to the particles after they have disintegrated.
“The particles will disappear, but some of their components will remain in the body,” says Mørch.
“We know that these may be toxic in high concentrations, so it is essential for us to find out how they affect both people and the environment after treatments.”
“The benefits must be greater than the drawbacks,” she stresses.
This new means of delivering drugs has already been successfully tested on mice and rats, and can open the way for entirely new treatments of brain diseases such as Alzheimer's and Parkinson's.
“We know that it's difficult to deliver drugs to the brain because it is surrounded by a very effective barrier which keeps the bloodstream and spinal fluid separate," Mørch says.
This barrier is designed to protect the brain as far as possible from potential harmful substances in the blood.
The researchers have now launched a trial with physicists at the Norwegian University of Science and Technology (NTNU). The aim is to find out what intensity of ultrasound is needed to get the gas bubbles to penetrate the barrier protecting our brains.
“If we succeed, it will then be possible to deliver drugs into parts of the body which we currently cannot reach,” says Mørch.


































