Sleep disturbance slips under the radar
As many as 40 percent of patients in the Norwegian mental health care system are likely to experience insomnia, but their sleep problems can be overlooked.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Either Norwegian mental health patients sleep very well, or something else is going on: when psychologist Håvard Kallestad examined more than 42,000 medical records of Norwegian mental health care patients for his doctoral disseration, he found exactly 34 primary diagnoses of insomnia.
That's less than one-tenth of one percent of the sample -- a vanishingly small number.
Kallestad believes the real number could be higher -- in some cases as much as 40 percent of patients themselves reported sleep problems, based on a sub-sample of patients whose doctors did not diagnose sleep disorders yet who actually said they had problems sleeping.
Kallestad studied sleep disturbance among mental health care patients and how these problems were recognised by health personnel. When he talked to doctors about the issue, he says, they reported that "people tend to think of sleep disturbances as a part of depression or anxiety rather than a separate problem meriting a diagnosis.”

Insomnia as a stand-alone problem
Kallestad's dissertation research also examined clinicians’ awareness of the consequences of insomnia among patients.
“I’ve lectured a lot to clinicians in mental health care about sleep disturbance. In each of these lectures I’ve asked how many had issued a diagnosis of non-organic insomnia and each time I was surprised by how few who had,” he said.
Non-organic insomnia is a sleep disturbance that is not directly caused by another health problem.
Kallestad says that recent research suggests that insomnia can be a stand-alone problem. It can be beneficially treated independently of other disorders.
However, a great deal of research has been conducted on groups who differ widely from patients who seek help from the mental health care system. Thus, Kallestad says, it’s questionable whether this research is relevant for people who are in treatment for psychiatric dysfunctions.
Different opinions
Kallestad studied patients who have been treated at psychiatric institutions and outpatient facilities. He and his colleagues looked into the diagnoses of about 42,000 patients – 93 percent of all the patients in mental health care during a period in 2008.
They also studied the degree to which more than 2,000 patients experienced problems with sleep. The reports on insomnia came from the patients themselves as well as from the clinicians involved in treating them.
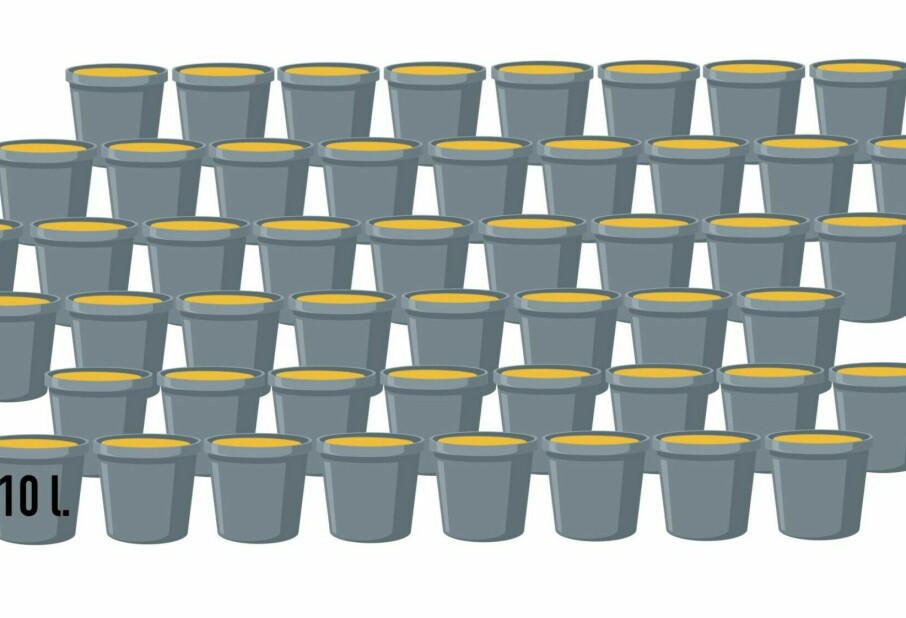
A surprisingly wide gap was revealed. Whereas some 40 percent of the patients reported experiencing sleep disturbance, their clinicians reported the problem in just 20-25 percent of the patients.
“We thought it was likely that the same patients who reported sleeping problems were the same ones listed by the clinicians. But it wasn’t so. Remarkably little overlap was found. We made the study among two different selections of patients and got the same results,” says Kallestad.
A problematic discrepancy
Kallestad can understand how patients might report sleep problems more readily than their therapists do.
However, he found a rather large group of patents whom health personnel thought suffered sleep disturbances even though these patients didn’t think so themselves. He has no good explanation for the disparity.
“This is just a mystery for me. I wish I had a good explanation,” he says.
Kallestad maintains that this discrepancy poses a problem, whatever the cause. Patients cannot be treated for insomnia if the clinician and the patient don’t see eye to eye on the problem. So he thinks therapists should be more diligent about querying patients about how well they their sleep and whether they wish they could sleep better.
“From earlier studies we know that patients don’t necessarily tell clinicians about their sleep problems, and clinicians often don’t ask. Another aspect is a lack of teaching about sleeping disturbances in the education of personnel for the mental health care system. It might not seem relevant to dig for a problem that you don’t know how to treat.”
Sleep is essential
The consequences can be serious if we are deprived of proper sleep for a long period. In his doctoral thesis Kallestad sought to ascertain how sleep disturbances affected patients.
More than 2,200 patients and their clinicians reported about quality of life, symptoms of other mental disorders and how much benefit the patients were getting from the treatment of these disorders.
It came as no surprise that patients with serious insomnia problems experienced a poorer quality of life and more serious symptoms of mental illnesses. They also benefited less from treatment of their psychiatric disorders.
“Sleep disturbances are important because a lot of patients are affected and the problems contribute independently to the severity of their illness,” says Kallestad.
Help available
Although Kallestad thinks few have learned enough about how to treat sleep disturbances, he points out these problems can and should be treated.
“Treatment of sleep disturbances is relatively simple. If it had been an issue which is hard to tackle, it would be less relevant. But a rather easy treatment is available,” he says.
Kallestad has gone through the limited existing literature on treatment of sleep disturbances among patients with mental health problems. This lack of information, Kallestad says, makes more research on treatment issues imperative.
He concludes, however, that if patients are offered targeted treatment for sleep disturbances, such as cognitive therapy, then an insomniac may also experience better results in the treatment of other mental health problems.
“Several studies on treatment of this patient group are required. We’ve now started a treatment study investigating the non-medicinal treatment of sleep disturbances among bipolar patients,” he says.
------------------------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling
Scientific links
- Differences between patients' and clinicians' report of sleep disturbance: a field study in mental health care in Norway
- Impact of sleep disturbance on patients in treatment for mental disorders