How does the flu virus work, and why do we have to make new vaccines every year?
ASK A RESEARCHER: To really answer this question, we have to dive into the microscopic world of viruses.
Having the flu can be just awful. But for some vulnerable groups it can be deadly.
A record number of Norwegians ended up in the hospital during the 2017/2018 flu season, and 1,400 of them died from influenza, according to the Norwegian Institute of Public Health.
What makes us feel sick is actually the result of how our body fights the virus, says Tone Gregers, a senior lecturer in biology at the University of Oslo.
“The body turns up its temperature, because that creates unfavourable conditions for viruses to multiply in our cells. The body also releases inflammatory substances which help kill infected cells. Eventually the body responds with a more long-lasting immune response,” says Gregers, who has also written a book on vaccines.
The flu vaccine also induces a long-lasting immune response.
But this response may not last all that long, because your immune system may not recognize the flu virus when it returns in the following year.
That’s because one virus can morph into many.
Sloppy propagation
“The influenza virus exploits a weakness in how it multiplies,” says Olav Hungnes, a senior scientist at the Norwegian Institute of Public Health and director of the WHO National Influenza Centre.
When the influenza virus propagates inside our body, a lot can change during the process, because the genetic material of the virus mutates very easily.
Many mutations can stop the virus from working. But as long as the virus is still able to attack our cells — and multiply inside them — many mutations provide an advantage.
“The influenza virus can change its outer surface and slip away from the immune system. That's why measles is a childhood disease, while we can get the flu many times during a lifetime,” Hungnes explains.
Influenza viruses also come in several different types. The viruses that make up each of these types can change from year to year.
Different genetic material
But what is it about the flu virus that causes it to mutate so often?
Part of the explanation lies in what its genetic material consists of, or how the recipe inside the virus tells it to multiply.
While viruses such as chickenpox and herpes have the same type of genetic material as humans — DNA — the flu virus relies on a different substance for its recipe.
“Influenza viruses are an RNA virus, and they mutate much faster," explains Bjarne Bogen, a professor of immunology at K.G. Jebsen Centre for Research on Influenza Vaccines at the University of Oslo.
“For other viruses that don’t change much, one vaccine will last a lifetime,” he says.
Mutates inside the body
As long as the virus is outside of the body, its inner recipe for propagation lies untouched inside a small capsule.
That means viruses can’t live or reproduce without hijacking another creature’s cells. For that reason viruses are not considered to be living.
But when a small virus capsule hits one of your cells, it clings to it and injects its genetic material. Then your cells think the virus's genetic material is your own.
The consequence is that your own cells do the virus’s job and create a bunch of new viruses.
That's when mutations occur.
“We have a flu virus that circulates throughout the year — either in the air or in humans. As long as the viruses can visit a host, they change,” says Gregers.
And there are especially many changes in RNA viruses, because their genetic material is more fragile than is found in DNA viruses.
Spikes on the surface
But to make this all the more confusing, measles also has genetic material that is composed of unstable RNA.
Nevertheless, we have good vaccines for this disease.
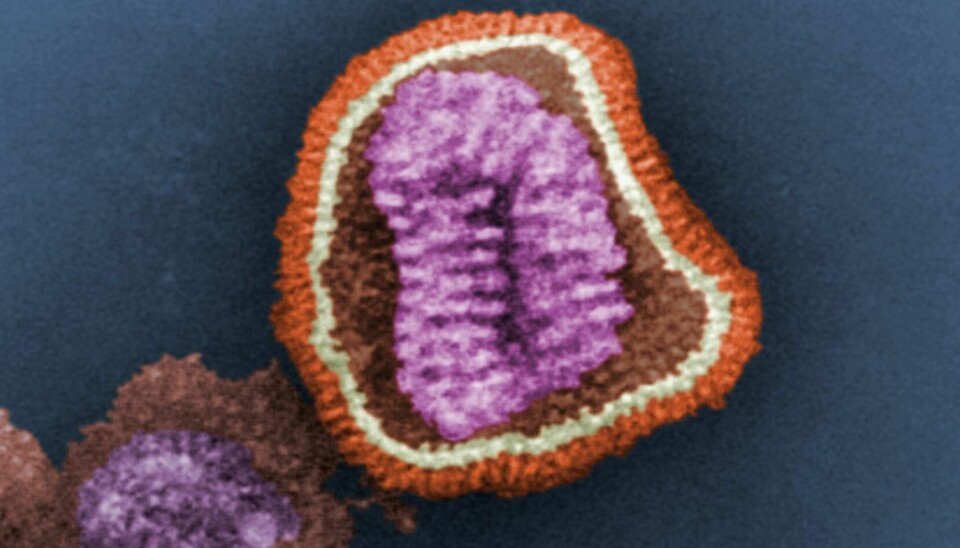
So to really understand what's so special about the flu virus, we need to look at the outside of the virus capsule that surrounds the virus’s genetic material.
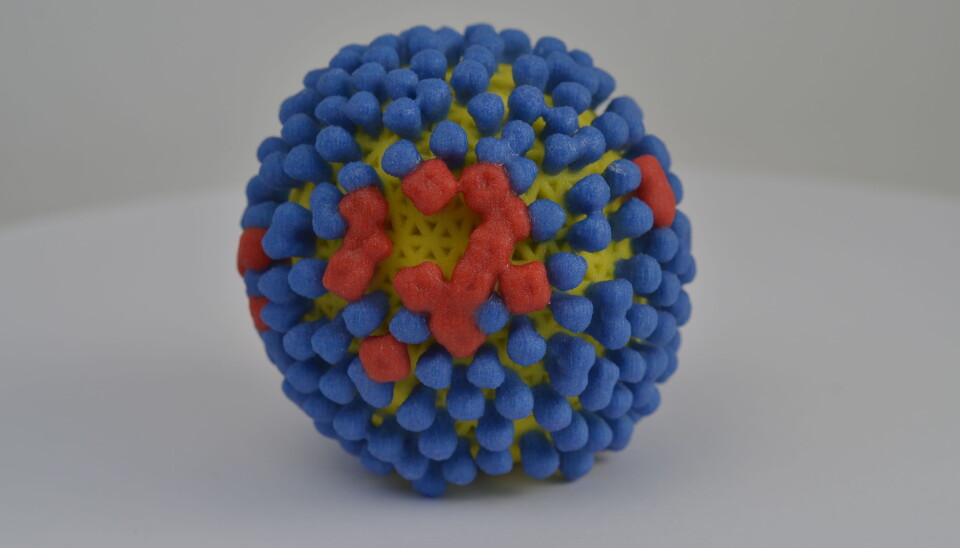
The capsule has proteins that act like spikes, and enable it to attach to our cells. And flu viruses are very flexible compared to other viruses.
"The influenza virus can withstand many more changes in the proteins that are on its surface than other cells," explains Hungnes.
In other words, the proteins on the capsule surface can change when the genetic material mutates, but they will still work. That enables them escape detection by our immune system, which has learned to recognize an old variant of the spikes.
The corresponding spikes on the outside of the measles virus, on the other hand, won’t function if there is a mutation.
Viruses from patients in Kansas and Phuket
Bogen is one of many scientists around the world who is working on a universal flu vaccine. This vaccine would last a lifetime, as opposed to today's vaccine, which has to be given anew every year.
But to achieve this, the vaccine must be prepared in a completely different way than today.
Today's flu vaccine is the result of a painstaking international collaboration between the authorities and pharmaceutical companies.
Vaccines contain killed viruses from ordinary patients from around the world. The vaccine for the 2019/2020 flu season contains viruses that originally came from four patients, one in Brisbane, one in Kansas, one in Colorado and one in Phuket.
These particular patients were chosen because they had the kinds of characteristics that researchers want from viruses that they’ll then turn into vaccines.
The job of the researchers is to predict which virus strains they think will infect most people during the coming flu season.
“Every season we have to make the best assessment of which virus strains are emerging and which can be a good candidate for creating a vaccine,” says Hungnes.
The Norwegian Institute of Public Health keeps track of which influenza viruses are infecting people in Norway. Hungnes himself has twice participated in the international meetings organized by the WHO, where it is decided which viruses should be part of the coming season's influenza vaccine.
Slow, painstaking production
The decision as to which viruses are most likely to spread has to be made long before the flu season begins. That’s because vaccine production is extremely slow and laborious.
And since viruses only multiply inside living cells, the way the vaccines are produced may be a little surprising to many.
“It usually takes at least half a year, because you have to grow the viruses in eggs, and it's a long and complicated process,” says Bogen.
The eggs inside of which the viruses multiply are common chicken eggs that have been fertilized.
Before ending up in the vaccine, however, the viruses from the eggs are killed or inactivated with chemicals.
A lot can change
And then it’s just a matter of crossing your fingers and hoping that the vaccine provides good protection. Unfortunately, a lot can change during the months it takes to produce the vaccine:
• Other influenza virus variants may end up being the dominant infectious agent.
• The flu viruses in the real world may have mutated so much that the vaccine does not provide protection.
• Influenza viruses may have changed in the laboratory during production.
The fact that the viruses mutate so easily is a big problem.
“Not only is it a problem that they mutate in the human body, but they can also mutate when you grow them in chicken eggs,” says Bogen.
If the viruses in the vaccine are different from those you are infected with, your immune system may not be able to recognize them.
Surface spikes key
But if the viruses change so much all the time, is there any hope of making a flu vaccine that provides lifetime immunity?
Bogen believes that the key to a universal flu vaccine lies on the surface of the viruses.
Our immune system can recognize the spikes on the virus, which are proteins that are called hemagglutinin.
Many of the scientists who are trying to make a new flu vaccine think the key is getting our immune system to focus on these spikes. So instead of injecting whole or large parts of the virus into the body, it may be enough to just use hemagglutinin in the vaccine.
A vaccine that makes itself
The way Bogen and his colleagues do this is to create a DNA fragment that contains the recipe for different variants of the spiked surface protein.
The idea is to create what is called a DNA vaccine. This kind of vaccine causes your body to create the substances that the immune system will learn to recognize.
The researchers have tested this type of DNA vaccine in mice. It contains the recipe for seven variants of hemagglutinin. Now they are testing vaccines with up to 18 different variants of the surface protein.
“The hope is that if we create broad immune reactions, you will be protected against new variants,” Bogen says.
The next step is to test the vaccine on humans.
But why not just include even more variants of the flu virus in the vaccines we make today?
Hungnes thinks that’s not a good idea.
“It’s demanding enough to produce an annual updated vaccine with four strains during the six months from when the strains are determined until the vaccine is ready. And we don't know how useful it would be for the immune response to get a jumble of related virus variants thrown at it at the same time,” he said.

Attacking bits that don’t change
Another strategy for making a universal flu vaccine is to concentrate on an even smaller portion of the virus. There are actually areas on the otherwise variable surface proteins that don’t change much.
“Some parts of the protein are more similar to other viruses in that they can tolerate change. Going for these parts could be closer to the holy grail that is the universal flu vaccine,” Hungnes says.
The US National Institutes of Health (NIH) is testing a vaccine for people using this particular strategy. The vaccine contains a small part of the spike’s surface protein that doesn’t change when the viruses mutate.
The Spanish Flu may have been a cross
The hope is that a new universal vaccine will also be able to provide protection against pandemics.
This is more than just a lofty goal: on a regular basis, an influenza virus from animals spreads to humans and creates a new worldwide flu pandemic. The most recent was the 2009 swine flu.
Bird flu and swine flu can be fatal to humans who get it, but these influenzas rarely infect other species.
But some of the worst pandemics we've had are due to a cross between human and animal viruses.
Both the Asian flu in the 1950s and Hong Kong flu in 1968-1970 were the result of this kind of crossover.
The Spanish Flu may also have been a mixed virus, according to the Norwegian Institute of Public Health.
These crossover viruses can occur inside an animal that is infected by both swine flu and human influenza simultaneously, as an example.
When viruses multiply inside one of the animal’s cells, a bit of the genetic material from both the bird flu and human influenza can end up in a new virus.
“It’s when you get a combination of genetic material from these different viruses that you get quite radically different viruses,” says Bogen.
If this kind of mixed virus can easily infect humans and causes serious illness, it can quickly lead to a new deadly pandemic.
———
This article is based on two articles on forskning.no:
Hva er det med influensaviruset som gjør at det endrer seg så fort?
Hva skal til for å lage en influensavaksine som gjør oss immune resten av livet?