This tiny sensor placed under the skin will measure the blood sugar levels of people with diabetes
The Norwegian sensor is to be coupled with Italian technology that administers insulin automatically. “If this is successful it will make life a lot easier for patients with diabetes”, says Norwegian doctor.
Bergen-based company Lifecare are behind the development of the sensor, which is to be injected into the skin of patients with diabetes type 1. Once in place, it will measure the levels of insulin. This information can then be sent to a smart watch or a phone.
The Norwegian company is now set to work together with European colleagues to develop a sensor and an insulin pump that can work together.
They are in fact making what they call a synthetic pancreas.
For most people, the pancreas regulates blood sugar levels automatically with its production of insulin. If you have diabetes type 1 your pancreas doesn’t work as it should.
The new technology aims to both measure blood sugar levels and administer insulin in the body when needed. Without any effort from the patient.
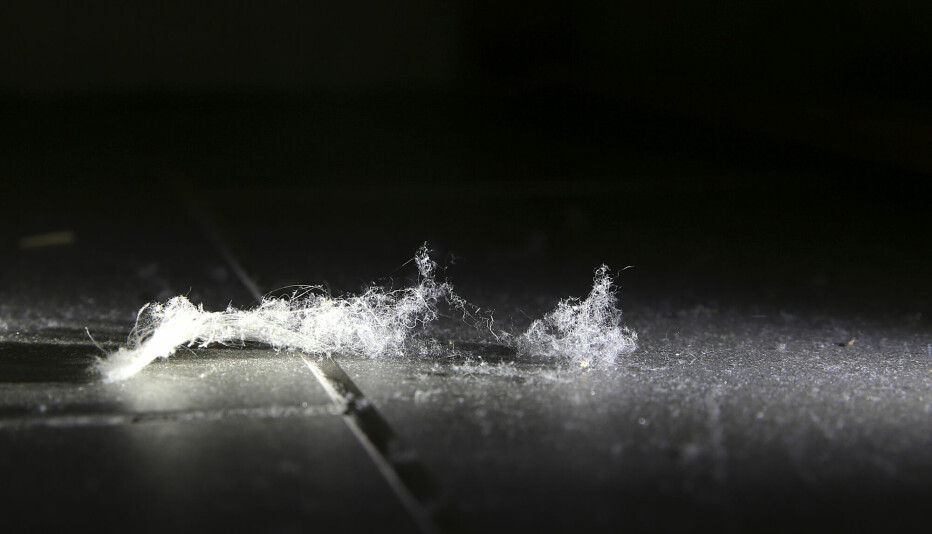
The size of a cell
The sensor is so tiny that it is nearly invisible.
“We have miniaturized the sensor to sizes that aren’t visible to humans”, says Rune Frisvold, Chief operating officer at Lifecare.
“It’s the size of a red blood cell”, he says.
For something so small to be able to measure anything, the company has used nanotechnology. With the help of a membrane, some electrodes and tiny amounts of liquid chemicals, the sensor can measure sugar levels in the tissue under the skin.
Good results in pigs
The sensor has been tested in the laboratory and showed good results on pigs. Next out are people with diabetes.
The researchers also have to find out which technology that works best in order to send wireless signals from the sensor under the skin.
And then finally, the goal of this European project is for the sensor to be coupled with an insulin pump being developed in Italy.
France and Germany are also part of the project, which goes under the name of Forgetdiabetes and has received a grant of 43 million NOK (just over 3,9 million Euros) in support from the EU.
The ambitious goal is for the artificial pancreas to be on the market by 2025.
Big and bulky sensors and pumps
Living with diabetes demands a lot from patients and their families.
Around 80 per cent of Norwegian children with diabetes already use some form of technology that measures their blood sugar levels continuously, as well as an insulin pump to administer insulin, according to Pål Rasmus Njølstad.
He is a professor and does research on diabetes at the University of Bergen and is a paediatrician at Haukeland hospital.
Still, many of these children will have to use needles to prick their fingers and measure blood sugar levels, in order to calibrate the technology. And the sensors also have to be replaced quite often. In addition, they are fairly big and bulky.
Njølstad therefore believes the miniature sensor has some real advantages to todays regimes.
“The fact that you can hide it under your skin is really great. Particularly for youngsters when it’s important for many to not be too different from their peers”, he says.
Has to be as precise as existing regimes
At the same time, he warns that there are a lot of things that have to work together in order for this new technology to replace todays sensors and pumps.
“You obviously cannot offer patients a treatment that gives poorer control of blood sugar levels than that which we have today”, he says.
Njølstad points to the fact that the miniature sensor does not measure blood sugar levels directly, but rather in the tissue under the skin.
“A challenge will be to be able to measure quick changes in the blood sugar for instance during a meal, or during physical activity”, says Njølstad.
It takes a few minutes from the blood sugar levels change until the sugar in the tissue changes.
According to Rune Frisvold from the Bergen-company Lifecare their technology will not differ from similar sensors already on the market. These are approved for measuring blood sugar levels as the delay is so small.
“If they succeed in what they say they wish to do, to integrate the sensor with a pump that controls the insulin levels automatically – then that would be quite fantastic”, says Kåre I Birkeland. He is an advisor for Lifecare, and also a professor at Oslo University Hospital.
“But there’s still a long way to go”, he says.
Translated by: Ida Irene Bergstrøm
———
Read the Norwegian version of this article on forskning.no