Is it possible to train the immune system to help in the fight against COVID-19?
Many experts have stated that we can’t do anything to improve the immune system's ability to cope with COVID-19. But research actually shows that training an ancient part of the immune system is possible. Could this be useful in future pandemics?
In the face of a pandemic, it’s tempting to look for any and all protective possibilities while we wait for a COVID-19 vaccine.
In recent months, various vitamins and other remedies have been recommended, and then immediately advised against by the experts. Numerous professionals in the field have been very clear that there is nothing we can do to boost the immune system, other than to avoid poor nutrition.
But this conclusion may be a bit too rigid.
Many of the recommended products are probably just bunk. But research does show that certain substances actually seem to be able to train the immune system to become better at fighting infections generally.
"There is a strong scientific basis for believing that inducing trained immunity preventively will ultimately play a significant role in strengthening the immune response to COVID-19", Anna Geller at the University of Louisville writes to sciencenorway.no.
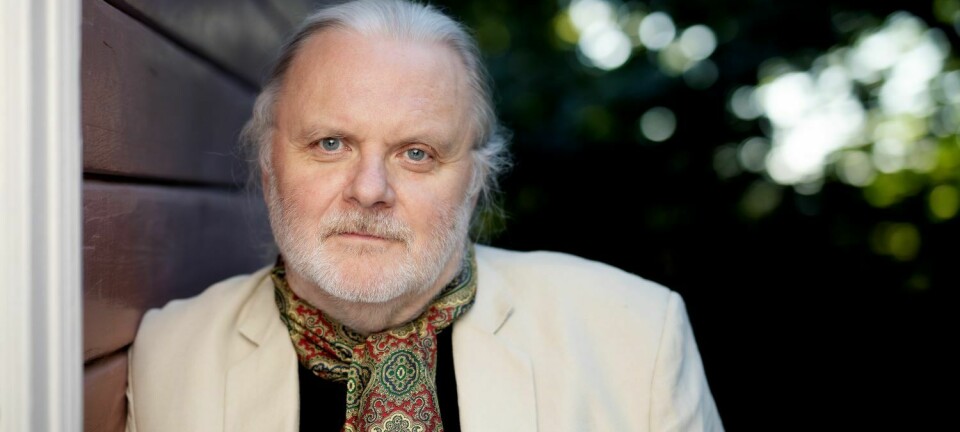
Jan Raa, a former professor at the University of Tromsø, is of the same opinion. He has long argued that training the immune system has received far too little attention.
A strange discovery
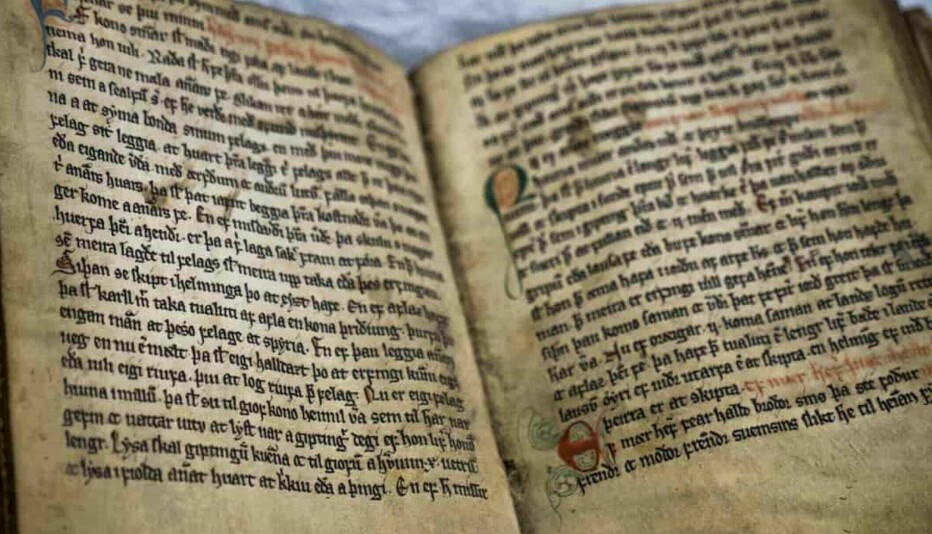
Some of the first hints are almost 100 years old.
Clues appeared in various places, including northern Sweden, where the tuberculosis vaccine was introduced for infants in 1927. Doctor Carl Näslund, who was responsible for the vaccinations, made a strange discovery.
The vaccine worked too well.
The mortality rate among the children who had received the vaccine was three times lower than usual. This was especially true in the first year of life, the age when many children died from diseases and infections.
Protecting against tuberculosis (TB) could not explain the astonishing effect, in part because this lung disease mainly took the lives of older children.
Näslund wondered if it was possible that the BCG tuberculosis vaccine stimulated a kind of immunity against completely different diseases.
He wasn’t alone.
Protection against illness?
In 1930, similar observations were made in Guinea-Bissau. Studies from several countries showed that vaccinated children were less likely to die from diseases such as malaria, sepsis, respiratory infections and leprosy.
The BCG vaccine has now been well documented to have this kind of protective effect. People who have been BCG vaccinated not only become immune to tuberculosis, but their immune system also gets better at fighting other bacteria and viruses.

An increasing number of studies also suggest that the phenomenon doesn’t just apply to the BCG vaccine and that certain substances, such as special types of beta-glucan (β-glucan), might have a similar effect.
Now more researchers are asking the question: Could this effect on the immune system protect against diseases like COVID-19? For example, could we prevent serious illness in this critical time window until scientists have developed a vaccine?
Immune system in two parts
It's all about our innate immune system.
The immune system, as we know, is our body's defence against foreign invaders such as viruses and bacteria.
The system consists of a number of different types of white blood cells – immune cells – that work to identify and neutralize invading microorganisms.
But the immune system consists of two parts, which work in quite different ways.
Our adaptive (or acquired) immune system is the part that learns to recognize diseases we have had and makes us immune to illnesses like chickenpox and rotavirus.
This defence happens when some of the immune cells change their DNA to specialize in recognizing a particular virus or bacterium. That way, the body can immediately counter this microorganism if we become infected again.
When a memory cell divides, the daughter cells inherit the DNA change. This is how the body can remember a disease year after year or sometimes a lifetime.
Vaccination stimulates the acquired immune system. By giving the body harmless bits of viruses or bacteria, the body can develop memory cells so that we become immune to the diseases without having had them.
This part of the immune system is really a new invention in evolution, says Raa, who has researched immune reactions in several species.
Biologically, the specialized immune system is a curiosity and is only found in about three percent of all animal species, he says.
What is found in all animals – from insects to mammals, including us humans – is the ancient innate immune system.
Innate immune system
Innate immunity is the first line of defence in the body, explains NTNU Professor Trude Helen Flo, who also does research on the immune system.
Immune cells in the innate immune system stand ready to respond to any intruder in the body. They secrete substances that inhibit viruses and bacteria from multiplying.
“The innate immune system deals with lots of bacteria and viruses every day, without you even noticing it,” says Flo.
This system is also indispensable when the body has more difficult things to deal with.
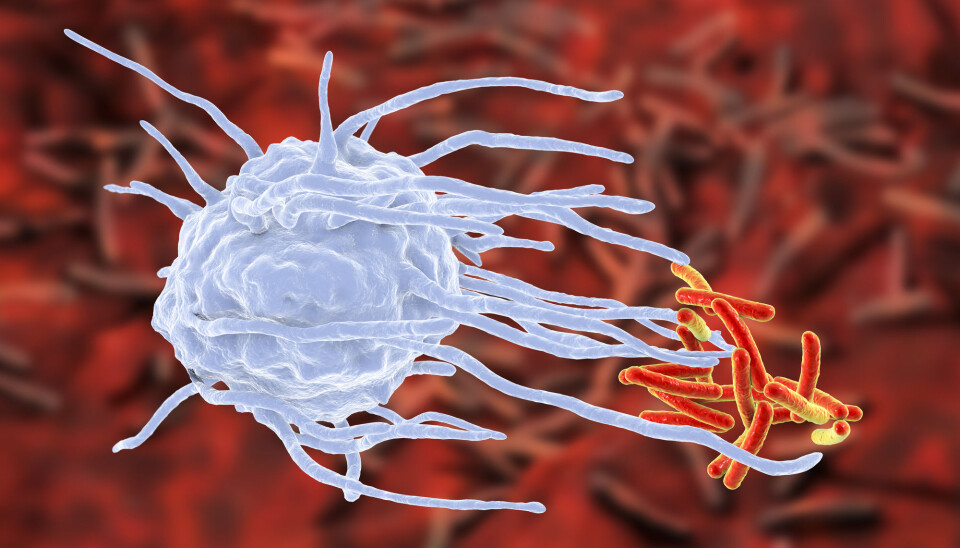
When you catch a flu or a cold, the innate immune system triggers the first response. But if that isn’t enough to beat back the infection, the body fires up the specific – or adaptive – immune system.
The cells from the innate system show the disease-causing microorganism to cells in the adaptive immune system. Then the specific system can begin to make specialized immune cells that can participate in a targeted attack on this particular microbe.
Capable of learning
The innate immune system is thus an absolutely necessary part of our defence. For a long time, scientists believed that our innate immunity wasn’t capable of learning or adapting and would respond in the same way every time, even in the face of microorganisms it hadn’t encountered before.
More recent research, however, has shown that this is not the case.
In fact, many indications show that the innate immune system gets better at coping with new challenges and can learn from past experiences.
“Things happen that cause the innate immune system to change its response when challenged again,” says Flo.
The DNA code itself doesn’t change like it does in the adaptive immune system, the professor says.
But when the cells in the innate immune system react to a threat, something does happen in the DNA. Parts of the tightly coiled DNA strand unfold so that the cell has access to the tools it needs to neutralize viruses and bacteria.
“In some cells, we’ve seen the DNA open up permanently. Then, when you get a new infection, there’ll be a stronger response,” says Flo.
Trained immunity suggested for COVID-19
Just a few years ago, Professor Mihail Netea of Radboun University named this phenomenon trained immunity.
Both Netea's and others' research suggests that such acquired immunity is behind the mysterious effect of the BCG vaccine. Thus, after tackling the BCG vaccine, the innate immune system responds more strongly and more purposefully to a variety of other infections.
Now Netea is advocating that we can use the BCG vaccine to prevent more diseases.
Already in May 2020, he and several colleagues proposed using the BCG vaccine and trained immunity in the fight against COVID-19 – not as a substitute for COVID-19 vaccines, but as an aid in the period before the vaccines are available.
"Induction of trained immunity by whole-microorganism vaccines may represent an important tool for reducing susceptibility to and severity of SARS-CoV-2" the research colleagues wrote in the scientific journal Cell.
Several studies have now been initiated to investigate the case, writes Netea in the New England Journal of Medicine in September 2020.
In addition, other researchers have argued for testing whether other live vaccines might have the same effect.
Researchers Paul Fidel and Mairi Noverr, for example, suggest investigating whether the MMR vaccine might be a simple and low-risk way to prevent COVID-19 deaths in vulnerable groups, in an article in the journal mBio.
A similar article by J. Wesson Ashford and colleagues came out in October.
Research has also been done suggesting that substances other than vaccines can train the innate immune system.
Raa and his colleague Rolf Seljelid from the University of Tromsø found just such a substance 40 years ago.
Beta-glucans
Raa and Seljelid found that a type of beta-glucan activates innate immunity in various animal species.
Beta-glucan is a type of fibre produced by a variety of plants, fungi and yeasts. There are many different beta-glucans, which have very different effects. The substance Raa and Seljelid found comes from baking yeast and is called beta-1,3/1,6-glucan.

Raa started a Norwegian industry to produce beta glucans for both animals and humans. The drug has now been used worldwide for several decades to prevent disease in domestic animals.
Raa and Seljelid argued early on that beta-1,3/1,6-glucan should be tested as a preventive medicine in humans.
They found little enthusiasm for the idea in Norway. But now international interest in beta-glucans appears to be increasing.
Beta-glucans suggested to boost immune system
Even before the corona pandemic began, American researchers wrote in the scientific journal Molecules:
“The question isn’t whether beta-glucans will move from being a dietary supplement to a generally accepted drug, but when.”
In July 2020 Anne Geller and Jun Yan provided new input from the University of Louisville. They believe beta-glucans hold strong potential to be used as a preventive medicine against COVID-19.
A lot of data suggests that beta-glucans can be an effective, inexpensive and safe way to help the immune system crack COVID-19, they write in Frontiers in Immunology.
However, the researchers are aware that more research is needed before the drug is approved for use. Studies done on beta-glucan in humans have shown mixed results.
These divergent findings are partly due to the fact that researchers were studying different types of beta-glucan.
The structure of the various beta-glucan molecules is of great importance for how the substance acts in the body. One type of beta-glucan might have a great effect, while another type has no effect.
More research needed
“I believe that our duty as researchers is to make sure that the treatment is safe and effective before we bring it to the public,” says Geller.
She believes it’s important not to hype up possible new treatments, such as what happened with the drug hydroxychloroquine.
One of the most important questions we need to answer is whether stimulating the immune system this way is harmful to our health.
The concern is timely. It is well known that an overactive immune system can do serious damage to the body.
Autoimmune diseases
Our immune system possesses powerful weapons. Used incorrectly, these weapons can harm us.
Autoimmune diseases, such as celiac disease, type 1 diabetes and Crohn's disease, are due to the immune system attacking the body's own cells. The immune system can also cause long-term inflammation, which can contribute to atherosclerosis, for example.
One study showed that patients who received the BCG vaccine and were later infected with malaria had more severe symptoms than unvaccinated patients, write Kristen A. Byrne and colleagues in Frontiers in Immunology.
A strong and active immune system is not always an advantage.

“I see all forms of treatment aimed at immune reactions as a pendulum,” Geller writes.
“There’s always a chance of leaning too far in the direction of overactivating the system.”
Geller still believes that trained immunity offers potential to prevent COVID-19. The effect of trained immunity seems to regulate more than it overactivates, she writes. This kind of regulation could, in the best case, prevent strong or misdirected immune reactions.
Possible balancing effect
Raa, on the other hand, has not seen any signs of serious side effects in any of the research on beta-1.3/1.6-glucan.
“If the innate immune system is activated and modulated in the right way, it’s possible to reduce the risk of dangerous bad reactions,” he says.
The immune system doesn’t necessarily react more strongly, but more correctly.
Netea concurs with Raa.
Netea and his colleagues recently published a study that showed that BCG vaccination improved the immune system’s ability to attack microorganisms, while at the same time causing less inflammation in the body in general.
“Research literature shows that by re-balancing the immune response, the BCG vaccine can actually have a protective effect against autoimmune diseases. But the studies are mostly done on mice,” he writes to forskning.no.
Don’t know how long it works
Another question is how long a possible protective effect lasts. Based on the mechanisms we know, it is probably a matter of a few months, but no one has reliable figures.
We also need to know more about when it is smarter to take vaccines or beta-glucans to achieve trained immunity. Geller believes this could be very important.
She points out that if you administer the dose after you’re infected, the risk of overactivation might be greater compared to inducing trained immunity prophylactically.
Could it be that the technique can both hurt and help, depending on when it’s used?
We still need to find out more about how the different substances work, like whether the BCG vaccine and beta-glucan have different effects or risks of side effects.
“No published studies have been done yet that compare these programmes for trained immunity, but we have unpublished data,” Netea says.
Interested but hesitant
So far, the effect of the BCG vaccine on trained immunity may be the better documented approach in humans. On the other hand, supplements with beta-glucan may be easier to administer. Beta-glucans also appear to have very few side effects.
“Beta-glucans have an extremely high safety profile. Few or no side effects for dietary supplements have been documented,” Geller says.
Professor Flo at NTNU, for her part, is interested but hesitant, both in terms of using trained immunity to prevent disease, and which substances may be best to use.
She believes a lot of research still needs to be done, especially when it comes to supplements with beta-glucans.
“You have to have bigger studies to find out which combination of beta-glucans works and what dosages are needed.
Like Geller, Flo believes that it is important not to give the public false hope.
“This isn’t a cure or a vaccine replacement, but it could reduce illness severity,” she says.
“Maybe trained immunity will become one of the measures at our disposal in new pandemics, as a contingency strategy while we wait for a vaccine,” Flo says.
Translated by: Ingrid P. Nuse
References:
P. Aaby & C. S. Benn, Saving lives by training innate immunity with bacille Calmette-Guérin vaccine, Proceedings of the National Academy of Sciences, 2012. Abstract.
M. G. Netea, Trained Immunity: a Tool for Reducing Susceptibility to and the Severity of SARS-CoV-2 Infection, Cell, May 2020. Abstract.
A. Mantovani & M. G. Netea, Trained Innate Immunity, Epigenetics, and Covid-19, New England Journal of Medicine, September 2020. Abstract.
P. L. Fidel & M. C. Noverr, Could an Unrelated Live Attenuated Vaccine Serve as a Preventive Measure To Dampen Septic Inflammation Associated with COVID-19 Infection?, mBio, June 2020. Abstract.
J. Wesson Ashford, MMR Vaccination: A Potential Strategy to Reduce Severity and Mortality of COVID-19 Illness, American Journal of Medicine, October 2020. Abstract.
R. Seljelid & J. Raa, Mobilisering av det mesenkymale infeksjonsforsvar, Tidsskrift for den norske legeforening, 2002.
V. Vetvicka, L. Vannucci, P. Sima & J. Richter, Beta Glucan: Supplement or Drug? From Laboratory to Clinical Trials, Molecules, March 2019. Abstract.
M. Del Cornò, S. Gessani & L. Conti, Shaping the Innate Immune Response by Dietary Glucans: Any Role in the Control of Cancer? Cancers, January 2020. Abstract.
A. Geller & J. Yan, Could the Induction of Trained Immunity by β-Glucan Serve as a Defense Against COVID-19?, Frontiers in Immunology, July 2020. Abstract.
K. A. Byrne, C. L. Loving & J. L. McGill, Innate Immunomodulation in Food Animals: Evidence for Trained Immunity?, Frontiers in Immunology, June 2020. Abstract.