Hormone spirals stand up to uterine cancer
Hormone spirals give protection against uterine cancer. The hormone spiral is superior compared to treatment with tablets.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Nearly ten years have passed since researchers at the University of Tromsø (UiT) first found that women who used contraceptive hormone spirals also get the benefit of a preventive effect against uterine cancer.
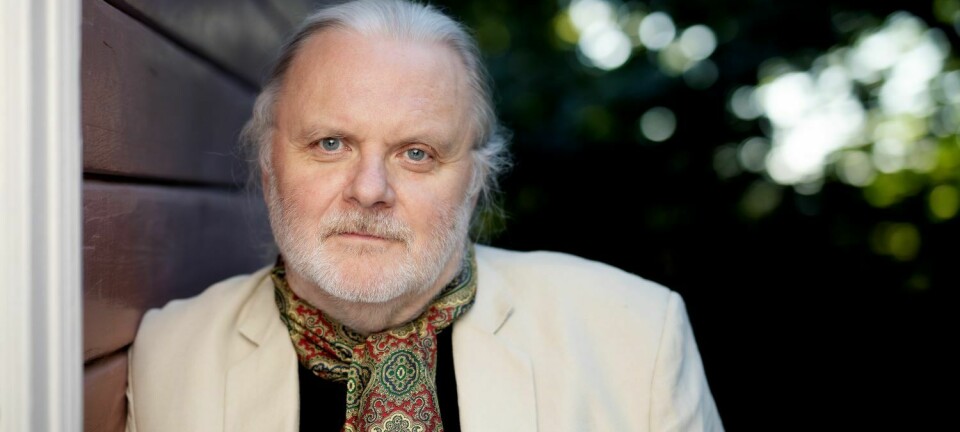
Now Anne Ørbo, a professor of gynaecology at UiT, reports that early stages of the cancer disappear in all the women in a group treated with the hormone spiral Mirena for six months, and later followed up for two years.
The women showed no indications of cell changes that can develop into malignant tumours as long they used the spiral.
Spiral is superior to tablets
The hormone spiral turns out to be superior to tablet treatment. The results are auspicious and the tendencies are clear: All the women in the group who used the spiral have responded.
“This means that the preliminary stages of uterine cancer abated completely with the use of the spiral,” says Ørbo, who is the first author of a new study, soon to be published in an international journal.
In need of national guidelines
A total of 170 women, all of whom had developed preliminary stages of uterine cancer, were followed up in a random control study.
This is a research method considered most appropriate for studying and comparing effects and forms of treatment.
Researchers have never before operated with such a long follow-up period of two years in studies of hormone spiral treatment versus tablet treatment.
The new results can lead to new national guidelines for the treatment of patients with early stages of uterine cancer.
Norway currently lacks common national routines. Progesterone in tablet form has long been a conservative method of treatment but hysterectomies have also prevailed, even among younger women.
“I’d say that far too many women have had hysterectomies," explains the professor. "Our results show that in the future we need to work differently. By selecting those with the highest risks and fitting them out with hormone spirals, we can reduce the number of cancer cases and surgeries.”
Returning when the spiral is removed
Ørbo has experienced that the hormone spiral makes dangerous mutations retreat on a cellular level. It isn’t clear yet which mechanism is at work in this context after the contraceptive device is put in place.
The results show that the positive effects of the hormone spiral last as long as the woman retains the hormone spiral in her uterus.
The professor thinks that the initial cancer stages are either reversed or that the mutations hide and are passive as long as the hormone spiral is active. Hormone spirals have to be replaced after five years of use.
“We indicate that when the spiral is removed, about 50 percent of the preliminary stage cancers return. It looks like women, especially those who are in risk groups for this type of cancer, should use this spiral continually to achieve a protective effect,” says Ørbo, who leads a research group on gynaecological cancers in Tromsø.
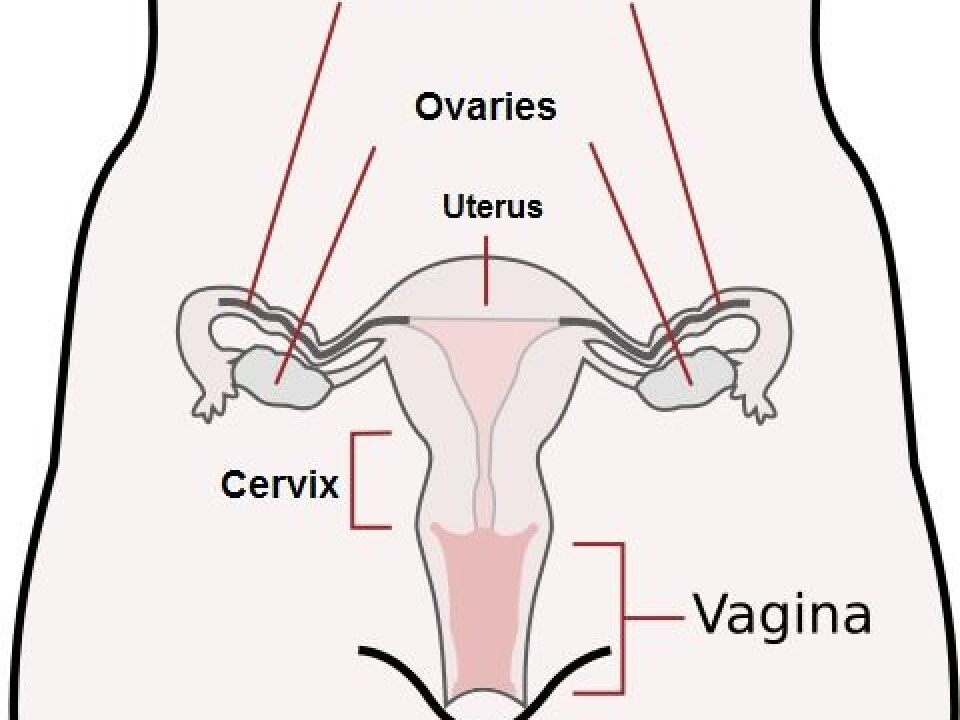
Upstaged by cervical cancer
Nearly all cases of uterine cancer develop from preliminary stages. Around 20 percent of these early-stage disorders develop into cancer.
Uterine cancer has been upstaged by cervical cancer, which is a different disease entirely. The HPV vaccine has been in focus as a preventive measure for the latter type of cancer.
In addition, cervical cancer can strike women even in their teens, while uterine cancer usually doesn’t develop until women are in their 60s.
Nevertheless, more women in Norway contract uterine cancer and it takes more lives. From 1999 to 2009 the number of cases of uterine cancer rose from 492 to 696.
By comparison, some 250-300 women are diagnosed with cervical cancer annually.
Obesity the largest risk factor
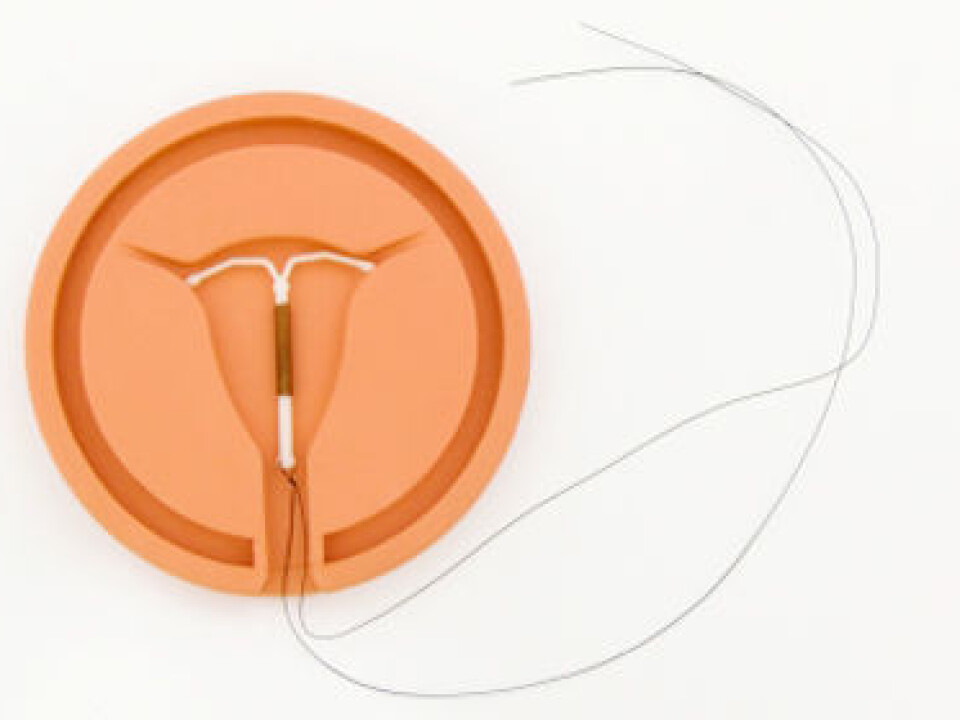
A hormone spiral works by releasing small doses of a synthetic hormone that has the effect of progesterone.
While increased levels of the female hormone oestrogen increase the risk of uterine cancer, progesterone helps the inner mucus membrane (endometrium) to contract and protects it from developing cancer.
Since uterine cancer starts in the uterus itself and is dependent on oestrogen, any factors that increase oestrogen levels in the body can also raise the risks of uterine cancer.
The biggest risk factor is linked to overweight. An obese woman has three times the risk of contracting uterine cancer.
“Metabolism disorders such as diabetes also raise the risk, as can high blood pressure, and also if women take oestrogen as a hormone supplement, or anti-oestrogens as a result of breast cancer,” says Ørbo.
Few side-effects
The professor says that only one percent of the women in the new study reported side-effects, such as irregular and at times excessive menstrual bleeding.
A total of 170 women, recruited from eight hospitals and nine gynaecological centres in the country, participated in the new study. It was conducted independently of all pharmaceutical companies.
One group used the hormone spiral, while two groups used tablets with different dosages.
The researchers witnessed reversals of the early stages of cancer among all the spiral users. In the tablet group with the lower dosage only half achieved this health gain.
In the tablet group using a higher hormone dosage there were many women who discontinued the treatment because of side-effects. So Ørbo and her colleagues consider this the least beneficial treatment form.
--------------------------------------------------
Read this article in Norwegian at forskning.no
Translated by: Glenn Ostling